While the findings of the 2019 trial (https://bit.ly/3roj1AI), testing add-on ibrutinib versus chemotherapy alone, were negative overall, Dr. Louis Staudt and his colleagues at the National Cancer Institute suspected that the drug had benefits for certain subsets of younger patients.
"My group had recently discovered a way to identify genetic subtypes of DLBCL and several of those had genetic alterations that suggested that they should respond well," Dr. Staudt told Reuters Health by phone. "Two of the genetic subtypes, MCD and N1, had truly an exceptional benefit from ibrutinib where their survival was 100% without evidence of disease at three years."
In comparison, patients who were treated with only rituximab plus cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) chemotherapy and a placebo had an event-free survival (EFS) rate of just 65% for MCD DLBCL and 55% for N1 DLBCL after three years, the researchers report in Cancer Cell.
They performed DNA and RNA sequencing on formalin-fixed and paraffin-embedded DLBCL tumors obtained from 773 of the 838 patients enrolled in the Phoenix trial, which had been restricted to individuals with non-germinal center B cell-like (GCB) DLBCL. Younger patients (< 60 years) made up 44% of the biopsied group.
Once DNA and RNA sequencing identified each tumor's mutations, translocations and gene-expression phenotypes, the non-GCB DLBCL biopsies were then assigned to genetic subtypes using the LymphGen algorithm created by Dr. Staudt and other members of NCI's Lymphoid Malignancies Branch.
Among the younger Phoenix trial patients, LymphGen was capable of identifying four genetic subtypes of non-GCB DLBCL: MCD, BN2, N1 and A53. For the study, 203 (26.3%) of these biopsies were classified, finding 110 MCD, 47 BN2, and 28 N1 cases, as well as 18 instances in which the tumor displayed genetic features of more than one subtype, removing these cases from consideration. A lack of DNA copy-number data prevented identification of any A53 subtype samples.
The subtype-defining genetic lesions were found in participants from different geographical regions, and both among younger and older patients in the Phoenix trial, "demonstrating the reproducibility of the genetic subtype assignments," the researchers note.
Both three-year EFS and overall survival (OS) estimates were 100% for the younger patients with MCD DLBCL (n=31) who received ibrutinib alongside R-CHOP. Those treated with R-CHOP alone, however, had significantly lower EFS and OS estimates, at 48% and 70%, respectively. This survival advantage linked to ibrutinib was consistent among patients from China and those from other countries.
Younger N1 DLBCL patients treated with ibrutinib and R-CHOP (n=13) also showed significant improvements with ibrutinib, with three-year EFS and OS of 100% compared with 50% for those receving R-CHOP only.
While younger patients with BN2 DLBCL (n=21) did not benefit from ibrutinib, various improvements were detected in all younger patients classified as having ABC DLBCL (n=239, 70.2%), a category based on gene-expression profiling rather than LymphGen classification.
"The take-home message from this paper is that separation of DLBCL into subtypes using advanced molecular testing can inform treatment," said Dr. Bonnie Harrington, an assistant professor at Michigan State University's College of Veterinary Medicine, in East Lansing, whose lab performs comparative studies on aggressive B-cell lymphoma in canine and human tissues.
"The biggest hurdle is financial," Dr. Harrington told Reuters Health by email. While she emphasized both the cost and lengthy computation time typically required for RNA sequencing, Dr. Harrington, who was not involved in the new study, expressed optimism for the development of a faster and potentially cheaper assay.
"Since we found this workaround to classify patients previously," she said, "I am certain that it is only a matter of time to find a way to sort patients into the current classification system."
Johnson & Johnson, which sells ibrutinib, supported the genetic tests and employed several of the authors. Dr. Staudt and his coauthors are listed as inventors on patent applications related to the research.
SOURCE: https://bit.ly/3x40FFD Cancer Cell, online November 4, 2021.
By Matthew Phelan
Posted on
Previous Article
« Artificial heart maker Carmat suspends implants due to quality issue Next Article
Lowering of CRC-screening age likely to affect colonoscopy demand, case mix, adenoma detection »
« Artificial heart maker Carmat suspends implants due to quality issue Next Article
Lowering of CRC-screening age likely to affect colonoscopy demand, case mix, adenoma detection »
Related Articles
August 5, 2021
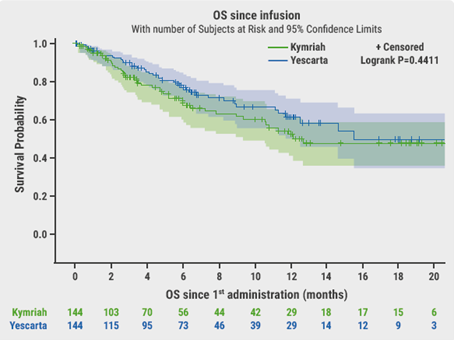
Promising chemo-free treatment options in r/r DLBCL
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

