https://doi.org/10.55788/1655ac74
The study, including 93 patients, categorised lipoprotein (LP) changes and the association between LP-Insulin Resistance Index (LP-IR) and hepatic steatosis following alcohol detoxification [1]. Patients that were enrolled in a 4-week alcohol detoxification programme at the National Institute of Health and with the last drink within 3 days of admission were registered.
Laboratory values and NMR LipoProfile Testing® were collected upon admission and during the first and third weeks. Fibroscan® with controlled attenuation parameter (CAP) was performed during the first, second, and fourth week. The Area Under Receiver Operator Characteristic (AUROC) was used to distinguish responders and non-responders, defined as a decrease or increase in liver CAP between week 1 and week 4.
A significant decrease was measured in CAP and aspartate aminotransferase over time. LP analysis showed a decrease in Apolipoprotein (Apo) A1 and an increase in ApoB and an initial decrease in LP-IR. A decrease in HDL particle number was detected, which was also seen in medium and large but not small HDL-P, as well as a decrease in HDL size. In comparison, an increase in LDL particle number was detected, with an increase in small and a decrease in large LDL particles, as well as a decrease in LDL size. Lastly, an increase in total triglyceride-rich LP particle number was observed.
As the liver is a key producer of ApoA1 and ApoB100, the authors hypothesised that with alcohol, ApoA1 is upregulated resulting in increased HDL and ApoB is downregulated, resulting in decreased LDL and triglycerides with lipids unable to leave the liver. Initial LP-IR was found to predict CAP improvement. Further studies are needed to elucidate the mechanisms of hepatic influx and efflux of lipids and the interplay between insulin resistance and alcoholic steatosis.
- Rapoport EA, et al. Adverse events in fecal microbiota transplantation: a systematic review and meta-analysis. Poster Su1602, Digestive Disease Week 2022, 21‒24 May, San Diego, CA, USA.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Normal BMI in NAFLD patients is associated with a higher risk of cardiovascular disease Next Article
Octreotide therapy beats standard of care in GIADs »
« Normal BMI in NAFLD patients is associated with a higher risk of cardiovascular disease Next Article
Octreotide therapy beats standard of care in GIADs »
Table of Contents: DDW 2022
Featured articles
Too much hygiene: CD in later life?
IBD
Antibiotic use elevates IBD risks in senior citizens
Too much hygiene: CD in later life?
Biologic treatment decreases dementia risk in senior IBD patients
CD: Induction treatment with upadacitinib successful in clinical and endoscopic ratings
IL-23 inhibition beneficial in maintenance treatment of UC
Positive outcomes for etrasimod in UC
Colonoscopy in UC: less pain and reduced recurrence with CO2 insufflation
Upper GI
Substantial increase of oesophageal cancer prevalence in the middle-aged
Cannabis users need more sedation medication for gastroscopy
Preterm delivery and NICU admission are associated with the development of eosinophilic oesophagitis
Dupilumab promising as treatment for eosinophilic oesophagitis
Other Highlighted Research
AI-assisted colonoscopy improves adenoma detection
Faecal microbiota transplantation: a safe procedure to treat recurrent Clostridium difficile infections
Oral microbes effective for prevention of recurrent Clostridium difficile infections
Octreotide therapy beats standard of care in GIADs
Improvement in hepatic steatosis but worse lipid profile after alcohol cessation
Normal BMI in NAFLD patients is associated with a higher risk of cardiovascular disease
COVID-19 increases the mortality rates of patients with ALD
Related Articles
March 21, 2022
Impact of COVID-19 on screening for colorectal cancer
July 18, 2022
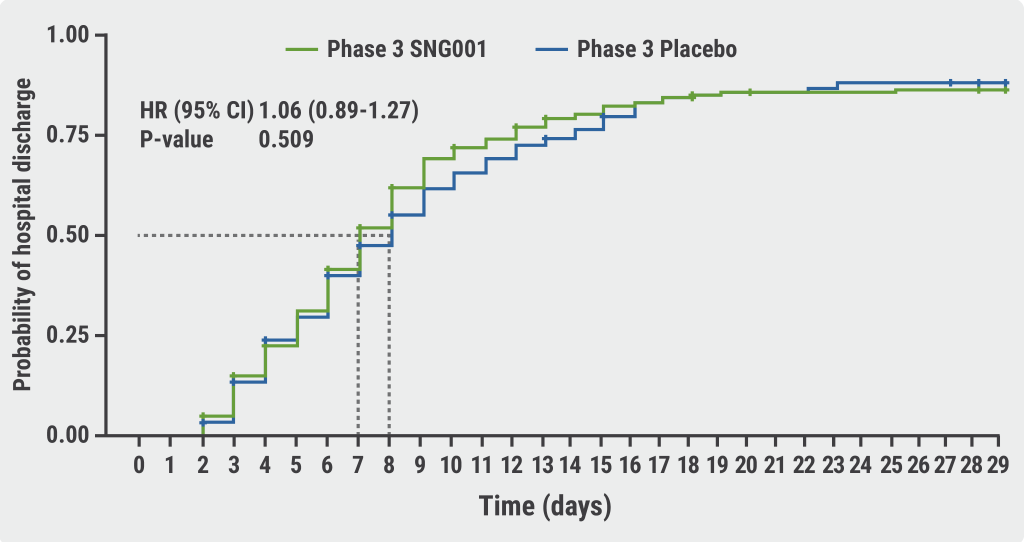
SPRINTER: SNG001 still in the running?
September 23, 2021
Robust support for COVID-19 vaccination in cancer patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

