https://doi.org/10.55788/158e209d
According to the new guidelines from the International Psoriasis Council, GPP should be defined as “a systemic disease characterised by cutaneous erythema and macroscopically visible sterile pustules” with the following subclassifiers:
- manifesting with or without systemic symptoms and signs;
- may or may not manifest with other types of psoriasis;
- can present as an acute form with widespread pustular eruption or a subacute variant with annular phenotype; and
- laboratory anomalies may or may not be present [2].
Essential diagnostic criteria for GPP include macroscopically sterile pustules on an erythematous base not restricted to the acral region or within psoriatic plaques. Supporting diagnostic criteria can include lakes of pus, painful skin, fatigue, fever, history of recurring flares, family history of psoriasis, elevated CRP, leukocytosis, neutrophilia, abnormal laboratory findings (i.e. hypocalcaemia, hyponatraemia, hypoalbuminaemia, abnormal renal or liver function tests), spongiform pustules of Kogoj on biopsy confirmation, and positive genetic findings (i.e. IL36RN mutation, MPO, AP1S3, SERPINA, CARD14).
Differential diagnosis
Psoriasis with pustules should not be classified as GPP. Acral pustules can present during flares and should not rule out GPP diagnoses; however, pustules that present only on acral lesions should not be classified as GPP.
GPP diagnosis should be distinguished from conditions such as acute generalised exanthematous pustulosis, pemphigus foliaceus, IgA pemphigus, and subcorneal pustular dermatosis [1]. Acute generalised exanthematous pustulosis presents following administration of medications, most commonly penicillins with numerous pin-point discrete sterile pustules, while GPP presents with widespread sterile pustules and lakes of pus. Facial pustular lesions occur commonly in acute generalised exanthematous pustulosis, while acral lesions are very rare. Finally, another distinguishing feature between acute generalised exanthematous pustulosis and GPP is the speed of onset and resolution: acute generalised exanthematous pustulosis has a rapid onset and resolution and does not relapse, while GPP flares can take 3 to 5 weeks and relapse.
Subcorneal pustular dermatosis presents with flaccid sterile pustules, which are absent in GPP, and does not present with facial and acral lesions. Another distinguishing feature is spongiosis, which is absent in subcorneal pustular dermatosis. Pemphigus foliaceus and IgA pemphigus can present similarly to GPP but histology and direct and indirect immunofluorescence (IgA deposits) can distinguish these diseases.
“GPP is a potentially life-threatening disease systemic inflammatory disease characterised by cutaneous erythema and macroscopically visible sterile pustule,” said Dr Choon. “The new International Psoriasis Council consensus on the definition and diagnostic criteria for GPP provides a clear and standardised framework for diagnosis.”
- Choon SE. Generalized pustular psoriasis: Definition and challenges. IFPA Conference 2024, 27–29 June, Stockholm, Sweden.
- Choon SE, et al. JAMA Dermatol. 2024. DOI:10.1001/jamadermatol.2024.0915.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Subcutaneous nivolumab may benefit patients across many indications Next Article
Towards prevention of psoriatic arthritis in patients with psoriasis »
« Subcutaneous nivolumab may benefit patients across many indications Next Article
Towards prevention of psoriatic arthritis in patients with psoriasis »
Table of Contents: IFPA 2024
Featured articles
Multiple novel oral agents show promise in psoriasis
Advances in psoriasis treatment: topical therapies show promising results
Personalised Medicine and Genetics in Psoriatic Disease
How close are we to personalised medicine in psoriatic arthritis?
Genetic and immunological advances in risk assessment and treatment of psoriatic diseases
Using advances in the genetics of psoriatic disease to better predict treatment response
Comorbidities and Complications in Psoriatic Disease
Depression complicates the management of psoriatic disease
The unfavourable role of obesity in psoriatic disease
Managing obesity and fibromyalgia in psoriatic disease
Advances in Psoriasis Treatment
Multiple novel oral agents show promise in psoriasis
Biologics for psoriasis: towards oral therapies and less frequent dosing
Advances in psoriasis treatment: topical therapies show promising results
Special Populations and Psoriatic Disease
Improving outcomes in pregnancy and psoriatic disease
Towards prevention of psoriatic arthritis in patients with psoriasis
Diagnostic Challenges and Disease Management
Itch and pain are major components of psoriatic disease and require management
Can diet help with the management of psoriasis?
Biologics in psoriatic arthritis: where we are and where we are headed
Related Articles
September 17, 2021
Bridging the gap between patients and access to psoriasis specialists
November 28, 2023
Dual IL-17 blockade yields efficacy on joints and skin
July 31, 2023
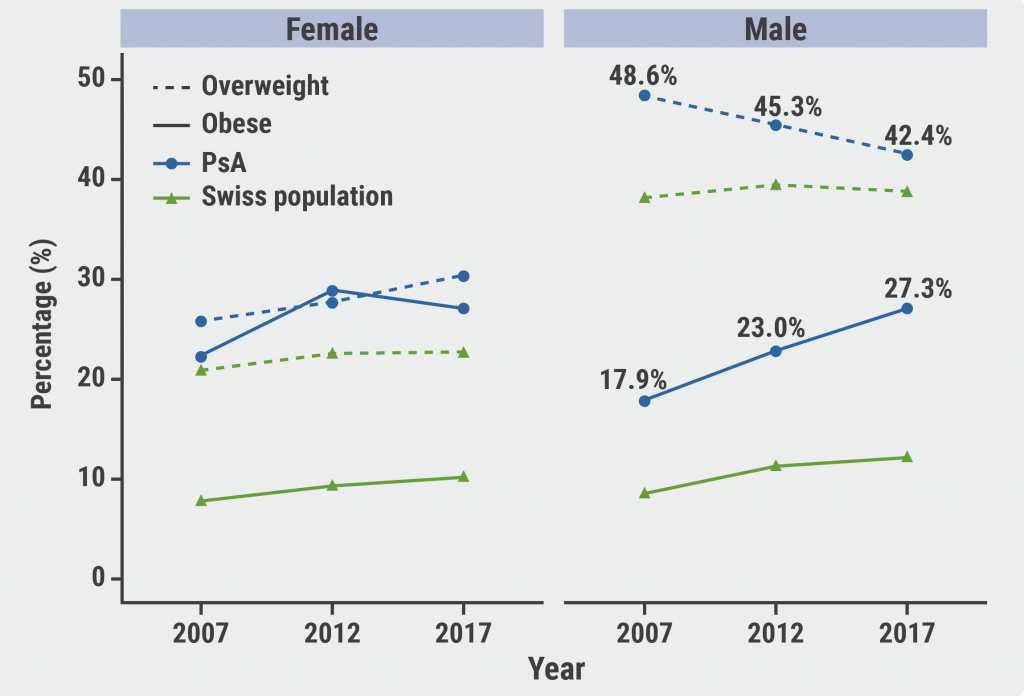
Obesity in PsA is increasingly affecting male patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

