"Anti-PD-1 agents have clearly improved outcomes for patients with melanoma. These treatments may cause long-term immune activation in both favorable and unfavorable (with autoimmune-like side effects) ways," Dr. Douglas Johnson of Vanderbilt University Medical Center in Nashville told Reuters Health by email.
"We found that chronic side effects were more common than previously recognized and affected a variety of often-overlooked organs, like the endocrine and salivary glands, joints, and peripheral nerves," he said. "Fortunately, these side effects usually caused minimal or mild symptoms, and were associated with improved treatment outcomes."
"Additional studies with longer follow-up to determine whether many of these side effects eventually resolve, as well as studies to quantify the impact on patient quality of life, should be done," he said. "Physicians should integrate this information when counseling patients on their therapeutic options."
As reported in JAMA Oncology, Dr. Johnson and colleagues analyzed data on 387 melanoma patients treated at eight academic medical centers between 2015-2020. The median age was 63, 61% were men, and all received adjuvant anti-PD-1 for stage III-IV melanomas.
Sixty-nine percent of patients had any acute irAE, defined as arising during anti-PD-1 treatment, including 19.5% with grades 3-5 events. One patient had neurotoxicity and one had fatal myocarditis.
Chronic irAEs - those that persisted beyond 12 weeks after anti-PD-1 discontinuation - developed in 43.2% of patients; most (96.4%) were grade 1 or 2 and only 14% had resolved by the last available follow-up.
irAEs that were particularly likely to become chronic were: endocrinopathies (83%), arthritis (48.9%), xerostomia (52.9%), neurotoxicities (73.3%), and ocular events (62.5%).
By contrast, irAEs affecting visceral organs (liver, colon, lungs, kidneys) had much lower rates of becoming chronic irAEs; for example, colitis became chronic in 13.6% of cases, two-thirds of which resolved with prolonged follow-up.
Age, gender, time of onset, and need for steroids were not associated with the likelihood of irAE chronicity.
Summing up, the authors state, "Patients treated with anti-PD-1 therapy increasingly experience long-term survival...We conclude that chronic irAEs, while usually low grade, occur more frequently than previously reported and particularly affect nonvisceral organs.
Dr. Badri Modi, a dermatologist who focuses on the identification and management of high-risk skin cancers at City of Hope in Duarte, California, told Reuters Health that the study "offers an important systemic examination of the irAEs that arise while on therapy and whether or not they improve after discontinuation."
"To my knowledge, this is the first study to try to characterize the longevity of immune-related adverse events," Dr. Modi said.
Although limited by its retrospective nature and small sample size, "this study should inform oncologists in how to better counsel patients about the long-term risks of using immune checkpoint inhibitors," he said by email. "While the study evaluates ICIs only in the case of adjuvant therapy for resected high-risk melanoma, these data can likely be extrapolated to other use scenarios for ICI in melanoma and other tumor types."
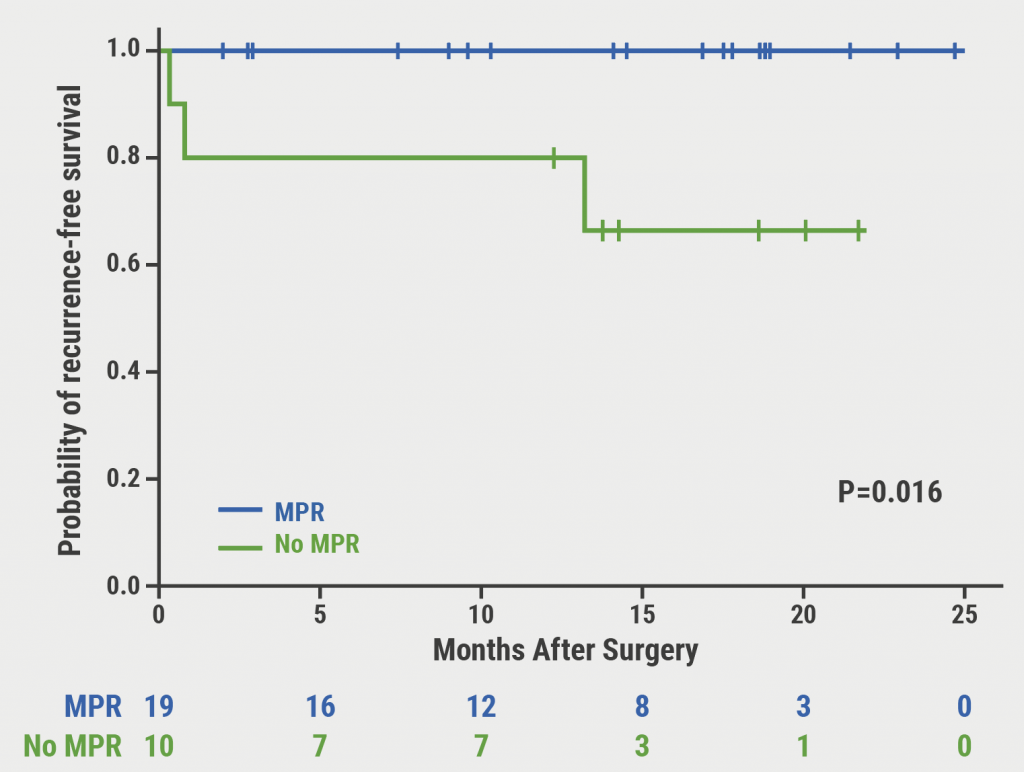
"Patients would benefit from understanding that unlike traditional medication side effects that abate after discontinuing the medication, some irAEs persist as chronic conditions," he said. "This knowledge can help patients make a more informed decision about choosing to pursue adjuvant therapy. This must be balanced with the understanding of improved relapsed-free survival offered by immunotherapy."
SOURCE: https://bit.ly/3mc9tns JAMA Oncology, online March 25, 2021.
By Marilynn Larkin
Posted on
Previous Article
« Infliximab reduces potency of first vaccine dose Next Article
Retinal changes may signal pre-clinical Alzheimer’s disease neuropathology »
« Infliximab reduces potency of first vaccine dose Next Article
Retinal changes may signal pre-clinical Alzheimer’s disease neuropathology »
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy