"Given the striking improvements that were observed in less severe HF in PARADIGM-HF (https://bit.ly/3qCX00i), we were very surprised by the results of the LIFE trial," Dr. Douglas Mann of Washington University in St. Louis told Reuters Health by email. "However, no matter how we analyzed the data, the trends did not favor treatment with sacubitril/valsartan."
"The results of the LIFE trial underscore the important differences that exist between patients with advanced HF, for which therapeutic options are limited, and less severe forms of HF with a reduced ejection, for which there are multiple treatment options," he said. "Thus, the results of the LIFE trial support the need for additional research in this patient population that is vastly understudied, and traditionally comprises <1% of large phase 3 clinical trials in HF."
The phase 4 trial was not statistically powered to observe differences in clinical outcomes between sacubitril/valsartan and valsartan, he noted.
As reported in JAMA Cardiology, 355 patients (mean age, 59.4; 73% men) with New York Heart Association class IV heart failure with a reduced ejection fraction were randomly assigned to receive sacubitril/valsartan (target dose, 200 mg twice daily) or valsartan (target dose, 160 mg twice daily) in addition to recommended therapy.
The trial began in 2017 and was stopped early due to COVID-19 risk.
The primary outcome was the area under the curve (AUC) for the ratio of NT-proBNP compared with baseline, during 24 weeks of therapy.
Seventy-two eligible patients (18%) could not tolerate sacubitril/valsartan, 100 mg/d during a short run-in period, and 49 (29%) discontinued the combination during the trial.
The median NT-proBNP AUC for valsartan alone was 1.19 versus 1.08 for sacubitril/valsartan. The estimated ratio of change in the NT-proBNP AUC was 0.95.
Compared with valsartan, the combination did not improve the clinical composite of number of days alive, out of hospital, and free from HF events.
A statistically significant increase in non-life-threatening hyperkalemia was seen in the sacubitril/valsartan arm (17% vs. 9%). No other safety concerns were observed.
Dr. Mann added, "One of the most important observations in the LIFE trial relates to the tolerability of sacubitril/valsartan in the advanced HF patient population. Less than 35% of the patients in LIFE were able to tolerate the high dose of sacubitril/valsartan that was used in the PARADIGM-HF trial."
Dr. Lynne Warner Stevenson, Director of Cardiomyopathy at the Vanderbilt Heart and Vascular Institute in Nashville, commented on the study in an email to Reuters Health. "The LIFE trial will have a major impact on treatment of patients both in and out of hospital, because it changes our current approach to prescribing sacubitril/valsartan in advanced HF. We were wrong to assume benefit in this high-risk population."
"While the benefits of sacubitril/valsartan are clear in robust patients carefully selected for the previous randomized trials," she said, "the TOLERABILITY of sacubitril/valsartan has been seriously overestimated."
"It took the LIFE trial to bring the lesson home that successful use of an angiotensin receptor II blocker - neprilysin inhibitor requires a sturdy blood pressure," she said.
"All trends in LIFE went in the wrong direction for sacubitril/valsartan," she noted. "The lack of benefit is not a power issue but a strong signal for caution. The risk for the endpoint of cardiovascular death and HF hospitalization was 1.32; cardiovascular death, 1.58; HF hospitalization 1.24; and patients had 11 fewer days alive without HF events if started on sacubitril/valsartan compared to valsartan alone."
"Just because neurohormonal modulation improves outcomes in stable outpatients does not mean that more is better when HF worsens," she said.
"If we had to define how LIFE changes our practice, perhaps it would be that we do not start sacubitril/valsartan in hospitalized patients who have recently had Class IV symptoms or borderline blood pressure. We may choose to wait until patients show clinical stability and sturdy blood pressure on other recommended therapies, and become more like the patients in the PARADIGM trial," Dr. Stevenson concluded.
Novartis provided the study drug and partial funding. Dr. Mann has an unpaid role on the company-sponsored PARADISE-MI trial, and four coauthors have received funds from the company.
SOURCE: https://bit.ly/3qtEGXz JAMA Cardiology, online November 3, 2021.
By Marilynn Larkin
Posted on
Previous Article
« New research upends principles of Parkinson’s disease onset Next Article
Biogen says Aduhelm lowers levels of second protein associated with Alzheimer’s »
« New research upends principles of Parkinson’s disease onset Next Article
Biogen says Aduhelm lowers levels of second protein associated with Alzheimer’s »
Related Articles
October 30, 2023
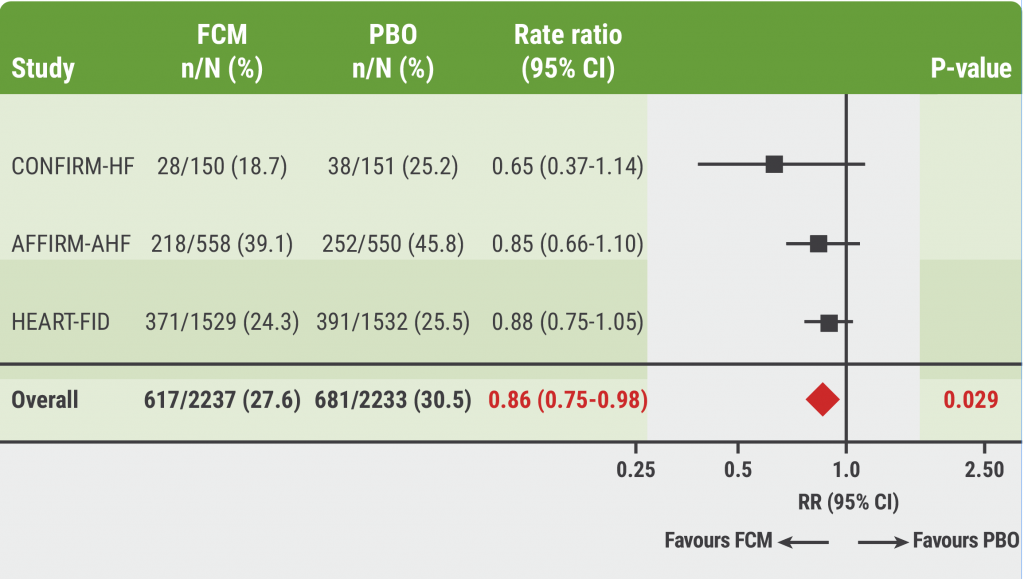
Meta-analysis: Does FCM improve clinical outcomes in HF?

November 28, 2022
AHA 2022 Highlights Podcast
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

