https://doi.org/10.55788/33436d08
Prompt identification, diagnosis, and treatment initiation in patients with de novo HF are needed to improve morbidity and mortality. Diagnosis is often delayed until echocardiography and specialist consultation is performed, which delays the provision of life-saving, evidence-based medication.
“This study aimed to look at the risk profile of people presenting with HF signs and symptoms and with an elevated NT-proBNP,” said Dr Lisa Anderson (St George’s Healthcare NHS Foundation Trust, UK) [1]. The researchers assessed changes in treatment and clinical events of 5,942 participants presenting to an outpatient clinic in Sweden with suspected HF and NT-proBNP levels >300 ng/L between 2015 and the end of 2020. This cohort was compared with 2,048 matched controls who presented for reasons unrelated to HF.
Overall, only 29% of participants with suspected de novo HF received a diagnosis of HF in the year following the index date. “The waits for echocardiography and diagnosis were very disappointing,” said Dr Anderson, “even in the group with the highest baseline NT-proBNP of over 2,000 ng/L.” Although Dr Anderson was impressed with the prompt NT-proBNP testing, which usually yielded a result within 24 hours, she found that changes in treatment were also suboptimal. In case of suspected HF, the use of loop diuretics almost quadrupled, but there was little increase in guideline-directed medical therapy, including prescription of beta-blockers, renin‐angiotensin system inhibitors, and mineralocorticoid receptor antagonists.
Compared with matched controls, participants with suspected HF had higher rates of HF hospitalisation and all-cause mortality (see Figure). The risks were high during the first weeks after the index and increased with rising NT-proBNP.
Figure: Risk of HF hospitalisation and all-cause mortality following suspected de novo HF [1]

HF, heart failure; PY, patient-years.
According to Dr Anderson, these findings highlight the need for a revolution in establishing a pragmatic ‘NT-proBNP rule-in’ approach to HF diagnosis to avoid the need to wait for phenotyping by echocardiography. She also advocated the adaptation of a low threshold for guideline-directed medical therapy initiation to improve morbidity and mortality in patients with suspected de novo HF. Further study is needed for an NT-proBNP rule-in approach to the diagnosis and management of HF.
- Anderson L, et al. Suspected de novo heart failure in outpatient care: high mortality and morbidity rates (REVOLUTION HF). Late-breaking clinical trials I, Heart Failure 2024, 11–14 May, Lisbon, Portugal.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Bio-ADM as a marker for congestion in patients hospitalised for acute HF Next Article
Algorithm-based remote patient monitoring was associated with lower mortality in a retrospective cohort study »
« Bio-ADM as a marker for congestion in patients hospitalised for acute HF Next Article
Algorithm-based remote patient monitoring was associated with lower mortality in a retrospective cohort study »
Table of Contents: HFA 2024
Featured articles
Meet the Trialist: Innovating cardiac monitoring with MONITOR-HF
Trials: Pharmacology
Effects of semaglutide on MACE irrespective of HF status
SEQUOIA-HCM: Aficamten demonstrates clinical efficacy in obstructive HCM
ARIES-HM3 trial: Subgroup analysis in patients with prior need for aspirin
Three diuretic regimens compared in the DEA-HF study
Adding a mineralocorticoid receptor modulator in heart failure with CKD
SGLT2 Inhibitors
Empagliflozin did not reduce mortality for HF after MI regardless of T2D status
SGLT2 inhibitors decrease atrial fibrillation risk in patients with HFrEF
SGLT2 inhibition: Major and early impact on heart failure hospitalisation risk
Trials: Other
Individualised diuretic titration in acute HF without a physician
Intravenous iron deficiency treatment improves exercise capacity in patients with HFpEF
CD34+ stem cells promote reverse cardiac remodelling after acute MI
Registries
Sex-specific outcomes and resource utilisation after HF hospitalisation
Application of guideline-directed medical therapy in patients with HFrEF in the Netherlands
Devices
PAP-guided management system appears safe in patients with HF
Delivery of CRT guided by non-invasive anatomy assessment
RELIEVE-ing HFrEF with interatrial shunting
Miscellaneous
Algorithm-based remote patient monitoring was associated with lower mortality in a retrospective cohort study
High mortality and morbidity in suspected de novo HF in outpatient care
Bio-ADM as a marker for congestion in patients hospitalised for acute HF
Hypertonic saline not effective in ambulatory patients with heart failure?
No effect of low-dose carperitide on mortality or hospitalisation in acute HF
Related Articles
August 19, 2021
Proenkephalin: A useful biomarker for new-onset heart failure?
January 14, 2022
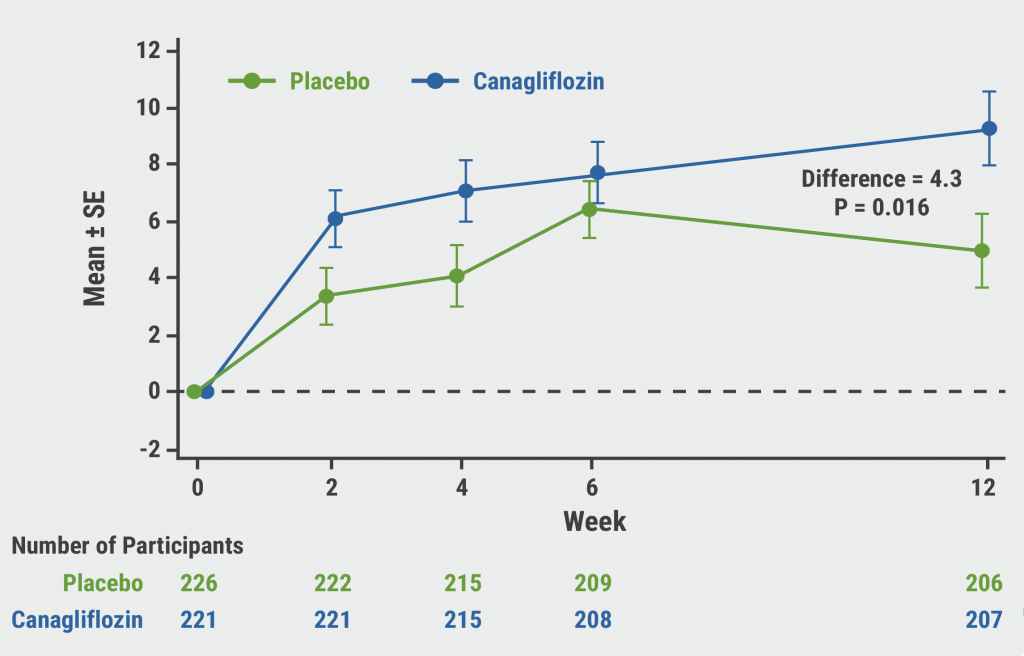
CHIEF-HF: Canagliflozin improves health status in heart failure
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

