The 2010 Task Force Criteria are the current gold standard to diagnose ARVC [2]. However, these criteria have not been tested to differentiate ARVC from athlete’s heart. In addition, they are not easy to assess in clinical practice as they require myocardial biopsy, genetic testing, morphology of ventricular tachycardia, and right-ventricular regional wall-motion abnormalities.
Dr Valentina Rossi (University Hospital Zurich, Switzerland) and colleagues evaluated whether atrial dimensions could be used to differentiate between both conditions, since the right atrium is often larger than the left atrium in patients with ARVC, even at an early stage, while atria enlargement follows a more symmetrical pattern in athlete’s heart [1].
This observational study included 21 ARVC patients and 42 athletes matched for age, gender, and BMI. The following echocardiographic, laboratory, and electrocardiographic parameters were included in the final score: indexed right/left atrial volumes (RAVI/LAVI ratio), serum NT-proBNP, RVOT measurements (i.e. PLAX and PSAX adjusted for BSA) on TTE, tricuspid annular motion velocity (TAM) on TTE, precordial electrocardiographic T-wave inversions, and depolarisation abnormalities according to the 2010 Task Force Criteria. A score ranging from 0 to 12 to differentiate ARVC and athlete’s heart was developed, with higher values suggesting ARVC (see Figure) [1].
Figure: Novel diagnostic score to differentiate between athlete’s heart and ARVC [1]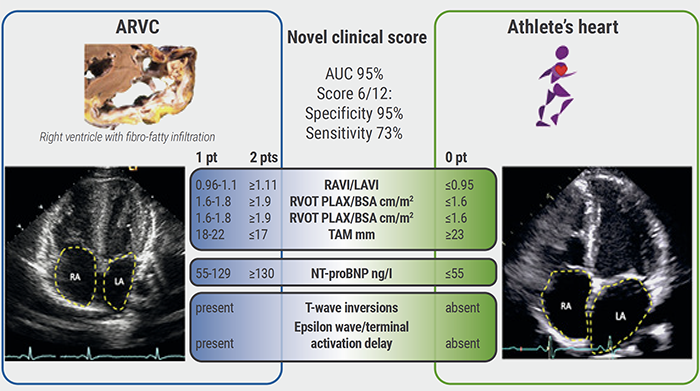
Parameters used in 2010 Task Force Criteria used the same cut-off. For newly introduced parameters (RAVI/LAVI, TAM mm, and NT-proBNP), cut-off values were calculated based on the ROC curves.
Figure kindly provided by Dr Rossi.
As per study design, the 2010 Task Force Criteria had the highest specificity (98%) and sensitivity (88%) to diagnose ARVC. However, those 2010 Task Force Criteria that are available in daily clinical practice (i.e. imaging, ECG) alone had a low sensitivity (41%; specificity 98%). In comparison, the proposed novel diagnostic score showed a sensitivity of 67% (specificity 91%) and thus outperformed the 2010 Task Force Criteria available in clinical routine (P<0.001).
The results from this study also showed that ARVC patients had a higher RAVI/LAVI ratio (1.78 vs 0.95; P<0.001), lower right-ventricular function (fractional area change 28 vs 42.18%; P<0.001; TAM 17.9 vs 23.3mm; P<0.001), and higher serum NT-proBNP levels (491 vs 44.8 ng/L; P<0.001).
Dr Rossi concluded: “Our diagnostic score including readily available clinical parameters improves sensitivity and can refine diagnostic work-up in daily clinical practice.” Due to the relatively small number of patients included, validation in larger cohorts should be sought.
- Rossi V. A novel diagnostic score to differentiate between athlete’s heart and ARVC. EHRA 2021 Congress, 23-25 April.
- Marcus FI, et al. Eur Heart J. 2010 Apr;31(7):806-14.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« The precordial R-prime wave: a discriminator between cardiac sarcoidosis and ARVC Next Article
EHRA Practical Guide on cardiac imaging in electrophysiology »
« The precordial R-prime wave: a discriminator between cardiac sarcoidosis and ARVC Next Article
EHRA Practical Guide on cardiac imaging in electrophysiology »
Table of Contents: EHRA 2021
Featured articles
Atrial Fibrillation and Direct Oral Anticoagulant
Predictors of young-onset atrial fibrillation
RACE 3 long-term results show fading benefit of targeted therapies in AF and HF
Deep dive into EAST-AFNET 4 results on early rhythm-control in atrial fibrillation
Cryo-FIRST study: improved AF and QoL outcomes with cryoballoon versus drug therapy
STROKESTOP: Benefits of systematic screening for atrial fibrillation
DOACs and bleeding: the role of antidotes
2021 EHRA practical guide: DOACs in pre-operative and bleeding patients
Atrial Ablation
Early rhythm-control ablation: insight from the CHARISMA registry
Personalised pulmonary vein isolation procedure feasible and effective
Pulmonary vein isolation: cryoballoon non-inferior to radiofrequency ablation
Diagnostic Tools
EHRA Practical Guide on cardiac imaging in electrophysiology
Novel diagnostic score accurately differentiates between athlete’s heart and ARVC
The precordial R-prime wave: a discriminator between cardiac sarcoidosis and ARVC
Limited added value of ECG-based mortality prediction in COVID-19 patients using machine learning
Devices
EHRA expert statement on pacemakers and intracardial devices: “watch out for the little old lady”
5-Year efficacy of subcutaneous implantable cardioverter defibrillator
Specific Populations
Individualised approaches key to success in resynchronisation therapy non-responders
Antiarrhythmic drug treatment in children: evidence-based recommendations
The importance of cardiac imaging in patients with congenital heart disease
Related Articles
June 16, 2021
Predictors of young-onset atrial fibrillation
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

