Prof. Jagmeet Singh (Massachusetts General Hospital, USA) presented treatment strategies for patients not responding to CRT [1]. Response can be assessed using hard measurements, remodelling, soft clinical measurements, and composite scores. As much as 43% of CRT patients are classified as non- or negative-responders after 6 months. However, responding is a continuum and a clear classification is often difficult. For example, 30-40% of patients can be mild responders and non-responsive in some way.
Determinants of CRT response include patient selection, lead implantation, device programming, and follow-up. For example, CRT in heart failure with narrow QRS complex increased mortality [2]. The considerable variability in electrical activation sequence as shown in endocardial maps may explain the variability in CRT response and argue against the one-size-fits-all ‘anatomical lead positioning’ strategy [3]. Furthermore, non-responsiveness is often multifactorial, with some of the factors not being directly related to CRT (e.g. suboptimal medication, comorbidities).
Individualised care using an integrated approach including heart failure, cardiac arrhythmia, and echocardiography services has been shown to significantly reduce the risk of mortality (see Figure). Optimisation of the devices, such as sound standard programming and use of automatic algorithms (e.g. AdaptivCRT, SMART-CRT, Respond-CRT, Synch-AV), also showed improved outcomes.
Figure: Improvement of event-free survival by multi-disciplinary CRT clinic versus conventional follow-up [4]
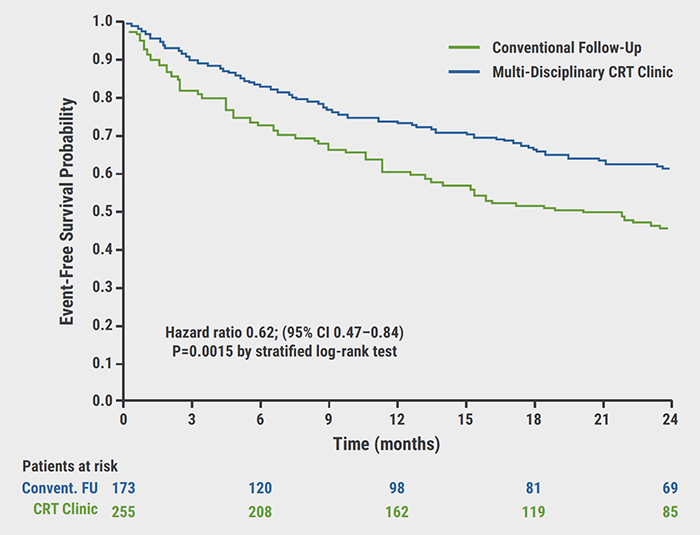
CRT, cardiac resynchronisation therapy; FU, follow-up.
Lead location has also been shown to contribute to clinical benefit. Apical left ventricular lead locations were associated with worse outcome irrespective of QRS morphology and electrical activation sequence, while targeting the most electrically delayed areas improved clinical outcome [5]. A study on multipoint pacing (NCT02006069) was recently stopped for futility, although multisite pacing was shown to be effective in some cases.
Prof. Singh summarised the importance of an individualised approach in CRT. Without selection of the right procedure for the individual at the beginning, non-responsiveness is likely. To gain relevant clinical benefit, treatment of non-responsiveness must also follow an individualised approach including medical optimisation, resolution of rhythm issues, AV optimisation, reassessment of lead location, and alternative pacing approaches.
- Singh J. How to treat cardiac resynchronisation therapy non-responders? EHRA 2021 Congress, 23-25 April.
- Ruschitzka F, et al. N Engl J Med 2013;369:1395-1405.
- Singh JP, et al. J Am Coll Cardiol EP 2020; in press.
- Altman R, et al. Eur. Heart J. 2012;33(17):2181-2188.
- Singh JP, et al. Circulation 2011:123:1159-1166.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Antiarrhythmic drug treatment in children: evidence-based recommendations Next Article
Novartis prostate cancer drug receives U.S. FDA breakthrough designation »
« Antiarrhythmic drug treatment in children: evidence-based recommendations Next Article
Novartis prostate cancer drug receives U.S. FDA breakthrough designation »
Table of Contents: EHRA 2021
Featured articles
Atrial Fibrillation and Direct Oral Anticoagulant
Predictors of young-onset atrial fibrillation
RACE 3 long-term results show fading benefit of targeted therapies in AF and HF
Deep dive into EAST-AFNET 4 results on early rhythm-control in atrial fibrillation
Cryo-FIRST study: improved AF and QoL outcomes with cryoballoon versus drug therapy
STROKESTOP: Benefits of systematic screening for atrial fibrillation
DOACs and bleeding: the role of antidotes
2021 EHRA practical guide: DOACs in pre-operative and bleeding patients
Atrial Ablation
Early rhythm-control ablation: insight from the CHARISMA registry
Personalised pulmonary vein isolation procedure feasible and effective
Pulmonary vein isolation: cryoballoon non-inferior to radiofrequency ablation
Diagnostic Tools
EHRA Practical Guide on cardiac imaging in electrophysiology
Novel diagnostic score accurately differentiates between athlete’s heart and ARVC
The precordial R-prime wave: a discriminator between cardiac sarcoidosis and ARVC
Limited added value of ECG-based mortality prediction in COVID-19 patients using machine learning
Devices
EHRA expert statement on pacemakers and intracardial devices: “watch out for the little old lady”
5-Year efficacy of subcutaneous implantable cardioverter defibrillator
Specific Populations
Individualised approaches key to success in resynchronisation therapy non-responders
Antiarrhythmic drug treatment in children: evidence-based recommendations
The importance of cardiac imaging in patients with congenital heart disease
Related Articles
June 16, 2021
Predictors of young-onset atrial fibrillation
June 16, 2021
DOACs and bleeding: the role of antidotes
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

