Based on available treatment guidelines, most patients who reach second-line therapy have already been exposed to lenalidomide [4,5]. “We are also going to see more patients who have been at least pretreated with or are refractory to daratumumab and bortezomib,” said Dr Gay.
How do we choose a suited subsequent therapy? “In my opinion, it is always better to switch drug class,” said Dr Gay [6]. Based on prior exposure to lenalidomide, proteasome inhibitors (PIs), or a combination of lenalidomide, PIs, and CD38-targeted therapies, subsequent lines can exist of therapies with a lenalidomide backbone, PI backbone, pomalidomide backbone, or novel immunotherapies [2].
Treatment selection must take into consideration several factors: disease-related factors (risk status, aggressiveness, renal disease), treatment-related factors (expected efficacy, time to first response, toxicity, need for dose reductions), and patient-related factors (age, frailty, performance status, comorbidities, organ function, patient preference) (see Figure) [2]. Next to these, use of prior therapies as well as response and toxicity should be considered [2].
Figure: Relevant parameters for treatment selection in RRMM patients [2]

AE, adverse events; LDH, lactate dehydrogenase; R-ISS, revised international staging system; R-MCI, revised myeloma comorbidity index.
Reprinted from Gengenbach L, et al. Cancers. 2021;13(17):4320. DOI:10.3390/cancers13174320, under the terms of the Creative Commons Attribution (CC BY) license.
Triplet combinations can be used after a first relapse, including PIs and/or immunomodulatory drugs and/or monoclonal antibodies [2]. Following a bortezomib- and dexamethasone-based first-line therapy (without lenalidomide or daratumumab), lenalidomide-dexamethasone-based regimens are recommended [2]. Lenalidomide-dexamethasone backbone therapies include daratumumab plus lenalidomide-dexamethasone (DRd; POLLUX) [7], elotuzumab plus lenalidomide-dexamethasone (EloRd; ELOQUENT-2) [8], carfilzomib plus lenalidomide-dexamethasone (KRd; ASPIRE) [9], and ixazomib plus lenalidomide-dexamethasone (TOURNMALINE-MM1) [10].
Patients refractory to lenalidomide can switch to bortezomib-dexamethasone (Vd)-, carfilzomib- dexamethasone (Kd)-, or pomalidomide-dexamethasone (Pd)-based regimens. Including for example, daratumumab plus bortezomib-dexamethasone (DVd; CASTOR) [11], carfilzomib plus daratumumab-dexamethasone (KdD; CANDOR) [12], Isatuximab plus carfilzomib-dexamethasone (IsaKd; IKEMA) [13], pomalidomide plus bortezomib-dexamethasone (PVd; OPTIMISMM) [14], and daratumumab plus pomalidomide-dexamethasone (DPd; APOLLO) [15].
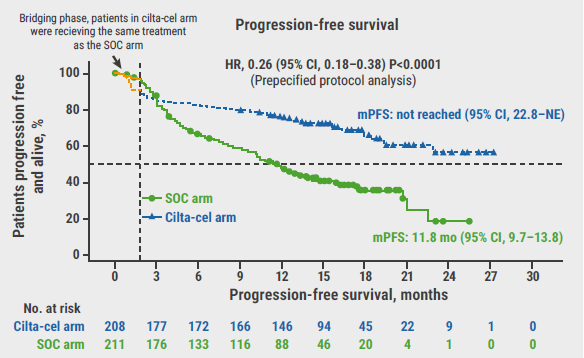
Ongoing trials in early relapse (≥1 prior lines) with novel therapies include B cell maturation antigen (BCMA)-targeted CAR T-cell therapies (ciltacabtagene autoleucel [cilta-cel] [16]), BCMA-targeted bispecific antibodies (teclistamab [17,18], elranatamab [19]), and GPRC5D-targeted bispecific antibodies (talquetamab [20]). The antibody-drug conjugate belantamab-mafodotin, previously available as a single-agent therapy, is currently under investigation in combination with bortezomib-dexamethasone and has shown positive results in DREAMM-7 [21].
“We have highly effective, novel triplets available in the treatment of relapsed/refractory multiple myeloma, also in the setting of lenalidomide-refractory patients,” concluded Dr Gray [2]. “The treatment choice is dependent on therapy-, tumour-, and patient-related factors and the new unmet need is double-refractoriness to immune modulatory agents and monoclonal antibodies and, in particular, this is addressed by new immune therapies which represent the new standard-of-care after the third line of therapy” [2].
- Ghandili S, et al. Oncol Res Treat. 2021;44(12):690-699.
- Gengenbach L, et al. Cancers. 2021;13(17):4320
- Gay F, et al. Treatment algorithm at first relapses. Session VI: RRMM patients. EMN 2024, 18–20 April, Turin, Italy.
- Dimopoulos MA, et al. Ann Oncol. 2021;32(3):309-322.
- Moreau P, et al. Lancet Oncol. 2021;22(3):e105-e118.
- Sonneveld P. Hematology Am Soc Hematol Educ Program. 2017;2017(1):508-517.
- Dimopoulos MA, et al. J Clin Oncol. 2023;41(8):1590-1599.
- Dimopoulos MA, et al. Blood Cancer J. 2020;10(9):91.
- Siegel DS, et al. J Clin Oncol. 2018;36(8):728-734.
- Richardson PG, et al. J Clin Oncol. 2021;39(22):2430-2442.
- Sonneveld P, et al. J Clin Oncol. 2023;41(8):1600-1609.
- Usmani SZ, et al. Blood Adv. 2023;7(14): 3739–3748.
- Marin T, et al. Blood Cancer J. 2023;13(1):72.
- Richardson PG, et al. J Clin Onc. 2018;36(15_suppl):8001.
- Dimopoulos MA, et al. Lancet Haematol. 2023;10(10):e813-e824.
- San-Miguel J, et al. N Engl J Med. 2023;389(4):335-347.
- Mateos MV, et al. J Clin Oncol. 2022;40(16_suppl):TPS8072.
- Touzeau C, et al. J Clin Oncol. 2023;41(16_suppl):TPS8067.
- Grosicki S, et al. J Clin Oncol. 2023;41(16_suppl):TPS8065.
- Cohen TC, et al. Blood. 2022;140(Supplement 1): 4418–4419.
- Mateos MV, et al. J Clin Oncol. 2024;42(36_suppl):439572.
Posted on
Previous Article
« Treatment choices beyond immunotherapy in relapsed/refractory multiple myeloma Next Article
Matters of the heart: late-breaking news from the American College of Cardiology »
« Treatment choices beyond immunotherapy in relapsed/refractory multiple myeloma Next Article
Matters of the heart: late-breaking news from the American College of Cardiology »
Related Articles
September 1, 2020
Higher risk of severe COVID-19 seen in people with blood cancers
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

