Rheumatoid arthritis (RA) and systemic sclerosis (SSC) patients weren't less likely to get invasive management than patients without AIRD, but like SLE patients, those with SSC were had higher mortality, Dr. Mamas Mamas and colleagues of Keele University, in Stoke-on-Trent, U.K., found.
"These are three very different populations with very different outcomes and risk factor profiles," Dr. Mamas told Reuters Health by phone. "We should be thinking of these rheumatic diseases as individual disorders."
AIRD is associated with an increased AMI risk, but it has not been clear if outcomes vary by disease subtype, Dr. Mamas and his team note in Mayo Clinic Proceedings. To investigate, they looked at National Inpatient Sample data on 6.7 million patients hospitalized for AMI in 2004-2014, 1.6% of whom had AIRD (RA, 1.3%; SLE, 0.3%; SSC, 0.1%).
SLE patients were significantly less likely than patients without AIRD to receive coronary angiography or percutaneous coronary intervention (PCI), with odds ratios of 0.87 and 0.93, respectively. And their risk of mortality (OR, 1.15) and bleeding (OR, 1.24) was significantly higher.
SSC patients were at significantly greater risk of major adverse cardiovascular and cerebrovascular events (OR, 1.52) and death (OR, 1.81). RA patients weren't at increased risk of complications.
RA is more common than other types of AIRD, and its effects on the cardiovascular system are better understood, Dr. Mamas noted. "I think cardiologists are much more comfortable in managing these patients, whereas I think that's less the case in SLE and definitely less the case in systemic sclerosis."
Patients with SLE are more anemic and at increased risk of renal failure and major bleeding, he said, and cardiologists may be reluctant to treat them invasively. But there are ways to reduce bleeding risk, according to Dr. Mamas, for example by performing PCI radially and abbreviating dual antiplatelet therapy.
"We know that patients with systemic sclerosis have coronary arteries that are diffusely diseased and tend to be smaller caliber, and that in itself makes it more challenging to treat such patients, particularly if you're going to try to treat them with a stent," he added.
"There is very little data on patients with systemic sclerosis and their outcomes following myocardial infarction," Dr. Mamas noted. "They have a worse baseline risk factor profile . . . and that will drive many of their adverse outcomes."
"Perhaps particularly for systemic sclerosis, we should be thinking about developing national registries of these patients where we can phenotype them much more granularly and follow them up and look at exactly what their outcomes are," he added.
Cardiologists should get rheumatologists involved early when caring for patients with AIRD, and treat AMI aggressively in these patients, Dr. Mamas concluded.
SOURCE: https://mayocl.in/2KeF2yc Mayo Clinic Proceedings, online November 26, 2020.
By Anne Harding
Posted on
Previous Article
« Circulating-tumor-cell dynamics have prognostic value in metastatic breast cancer Next Article
Nomogram could predict treatment-induced hearing loss in head and neck cancer »
« Circulating-tumor-cell dynamics have prognostic value in metastatic breast cancer Next Article
Nomogram could predict treatment-induced hearing loss in head and neck cancer »
Related Articles
September 4, 2019
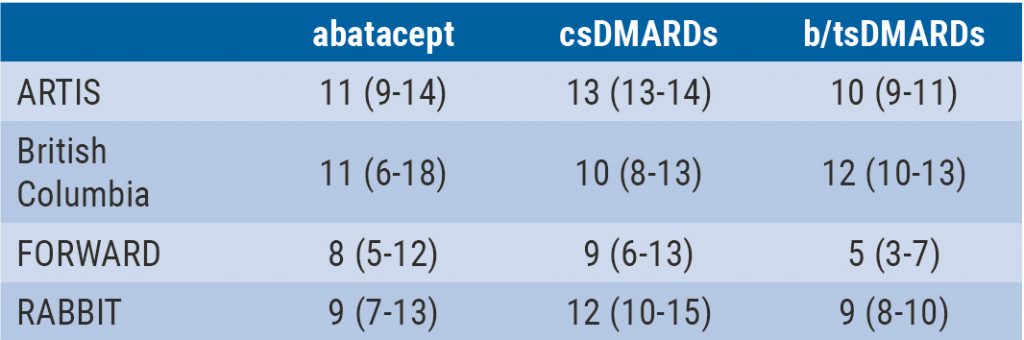
Integrated 10-year analysis confirms safety profile abatacept
January 18, 2021
How to choose imaging modalities in large vessel vasculitis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

