https://doi.org/10.55788/8b8211a9
“An intracoronary, imaging-defined vulnerable plaque tends to increase major adverse cardiac events, and OMT is the standard approach to stabilise the vulnerability of the plaque,” Prof. Seung-Jung Park (University of Ulsan College of Medicine; Asan Medical Center, South Korea) explained [1]. The multicentre, randomised-controlled PREVENT trial (NCT02316886) compared OMT alone with OMT plus preventive PCI of vulnerable non-flow-limiting coronary plaques [1,2].
The 1,606 participants from research hospitals in South Korea, Japan, Taiwan, and New Zealand were randomised 1:1 to PCI and OMT or OMT alone. Among the inclusion criteria were stenosis >50% and a negative fractional flow reserve (FFR) of ≥0.80. The primary endpoint was a composite of death from cardiac causes, target vessel myocardial infarction (MI), ischaemic-driven target vessel revascularisation, or hospitalisation for unstable/progressive angina, summarised as target vessel failure at 2 years.
The results showed a cumulative incidence of target vessel failure in 0.4% of the OMT plus PCI arm, compared with 3.4% on OMT alone (see Figure). This resulted in a significant HR of 0.11 (95% CI 0.03–0.36; P=0.0003). After a longer follow-up at 7 years, a consistent advantage of preventive PCI was seen with target vessel failure rates of 6.5% versus 9.4%, respectively (HR 0.54; 95% CI 0.33–0.87; P=0.0097).
Figure: Target vessel failure at 2 years of follow-up in the PREVENT trial [1]
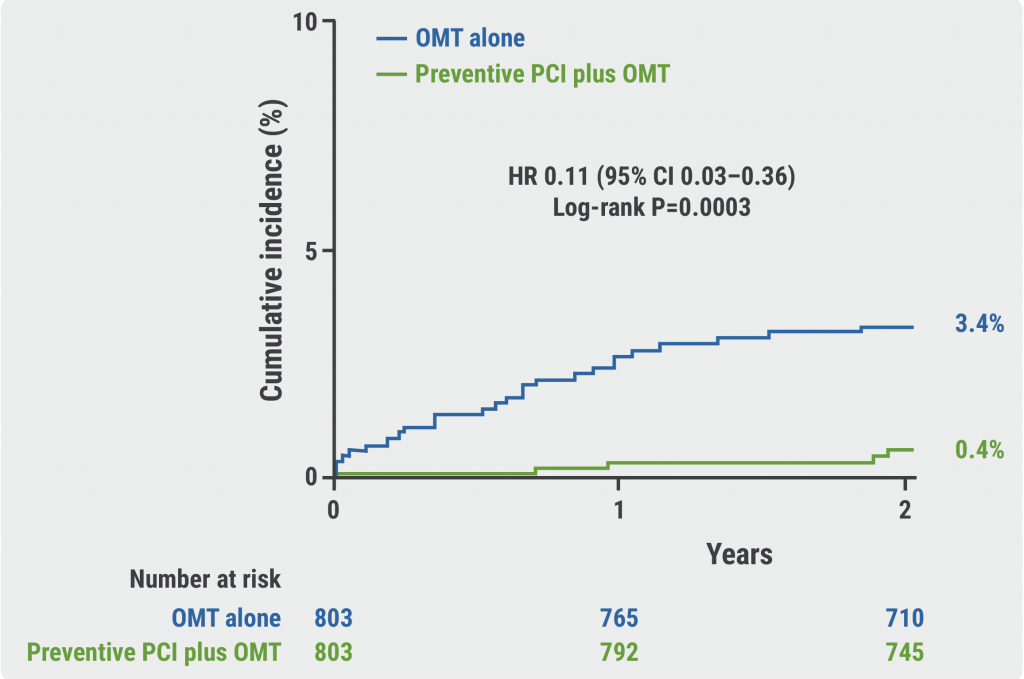
CI, confidence interval; OMT, optimal medical treatment; PCI, percutaneous coronary intervention.
Furthermore, the composite of any-cause death, any MI, or any repeat revascularisation through 7 years was significantly reduced in the intervention group (HR 0.69; 95% CI 0.50–0.95; P=0.022). Among the individual primary outcome components, only ischaemia-driven revascularisation and hospitalisation for angina were significantly in favour of the PCI group, other components showed no between-group difference. Also, no statistical differences were determined for secondary endpoints like bleeding events and stroke.
“Our key findings might provide a novel insight into the role of a preventive PCI on non-flow-limiting high-risk vulnerable plaques in the future,” concluded Prof. Park. Further information with regard to the definition of optimal medical therapy in this open-label trial may shed further light on the efficacy and safety of this strategy.
- Park SJ. Preventive PCI or medical therapy alone for atherosclerotic coronary vulnerable plaques. LB5, Session 412, ACC 2024 Scientific Session, 6–8 April, Atlanta, USA.
- Park SJ, et al. Lancet 2024; April 8. DOI: 10.1016/S0140-6736(24)00413-6.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« KARDIA-2: Add-on zilebesiran effectively lowers blood pressure Next Article
Meet the Trialist: Innovating cardiac monitoring with MONITOR-HF »
« KARDIA-2: Add-on zilebesiran effectively lowers blood pressure Next Article
Meet the Trialist: Innovating cardiac monitoring with MONITOR-HF »
Table of Contents: ACC 2024
Featured articles
Matters of the heart: late-breaking news from the American College of Cardiology
Heart Failure and Cardiomyopathy
STEP-HFpEF DM: Semaglutide beneficial in patients with HFpEF and diabetes
IMPROVE-HCM: Promising results for ninerafaxstat in non-obstructive HCM
Acute Coronary Syndrome and Acute Myocardial Infarction
ACS: Necessary DAPT after PCI may be shorter than currently advised
AEGIS-II: ApoA-1 did not reduce MACE in patients with myocardial infarction but may provide benefit in patients with high LDL levels
REDUCE-AMI: Re-evaluating the role of routine beta-blockade in patients with acute myocardial infarction
Interventional Cardiology in 2024
Self-expanding versus balloon-expendable TAVR in patients with small aortic annuli
Safety of TAVI non-inferior to SAVR for patients with lower surgical risk
Interatrial shunt for HF: neutral primary endpoint but potential benefit in HFrEF
Peripheral artery disease: procedure-guidance by IVUS superior to angiography
IVUS-guided PCI beats angiography in patients with acute coronary syndrome
Addressing frailty in patients undergoing TAVR
Novel Developments in Risk Factor Management
Preventive PCI of vulnerable intracoronary plaque leads to favourable outcomes
KARDIA-2: Add-on zilebesiran effectively lowers blood pressure
BRIDGE-TIMI 73a: Olezarsen halves triglyceride levels
Plozasiran: A novel approach to severe hypertriglyceridaemia
High-risk and very high-risk patients meet LDL-cholesterol targets with lerodalcibep
No cardioprotective effect of ACE inhibitors in patients with cancer
Best of Posters
SGLT2 inhibition in heart failure more advantageous for women than men
Anxiety and depression: Lifestyle influential in MACE prevention
Meet the Trialists
Related Articles


November 28, 2022
AHA 2022 Highlights Podcast
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

