An analysis from MAIA based on frailty scores showed that the addition of daratumumab to lenalidomide and dexamethasone (Rd) leads to a maintained PFS benefit across frailty subgroups (non-frail and frail). However, frail patients tended to derive lower benefits compared with their non-frail counterparts with both D-Rd and Rd regimens [3]. Furthermore, MAIA also showed a trend for increasing Grade 3/4 adverse events, infections (driven mostly by pneumonia), as well as treatment discontinuation rates with increasing frailty with both D-Rd and Rd [3].
With these data in mind, it’s time for a paradigm shift in how patients are managed, according to Dr Manier. Instead of using one regimen for all patients, the aim should be to improve minimal residual disease (MRD) negativity rates for fit patients, while aiming to provide the lowest toxicity rates for frail patients [2].
The results from the phase 3 IFM2017-03 trial can offer a steroid-sparing alternative for frail participants with newly diagnosed transplant-ineligible multiple myeloma. Participants were randomised to either lenalidomide dexamethasone (Rd) or daratumumab lenalidomide (DR). After 12 months of treatment, 42% and 58% of participants in the Rd and DR arms respectively, had a very good partial response or complete response (P=0.013). A trend was observed for higher rates of MRD negativity with DR compared with Rd, at the expense of more haematological toxicities in the DR arm (neutropenia Rd 15% vs DR 44%; P<0.001; anaemia Rd 2% vs DR 11%; P=0.01) [4].
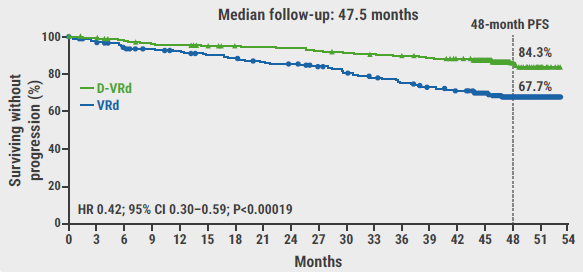
What other trials can inform treatment decisions of elderly patients? Quadruplets are being assessed in several phase 3 trials including IMROZ (Isa-RVd vs RVd, NCT03319667), CEPEHUS (Dara-RVd vs RVd, NCT03652064) and BENEFIT (Isa-VRd vs Isa-Rd, NCT04751877). CAR T-cell therapy is also being assessed as part of the CARTITUDE-5 trial (NCT04923893, VRd followed by either cilta-cel or Rd), while MAGNETISMM-6 (NCT05623020) and MajesTEC-7 (NCT05552222) are assessing the role of bispecific antibodies.
Regardless of therapy, patients should still receive supportive care consisting of infection prophylaxis (immunisation, antiviral and antibiotic use, IVIG if needed, monitoring), treatment of bone disease, palliative care as well as physiotherapy and rehabilitation medicine.
Dr Manier ended the presentation with his personal opinion on treatment adaptation. The one-size-fits-all approach using the D-Rd regimen in patients with transplant-ineligible multiple myeloma should be adapted. Using simplified frailty scores and cytogenetic risk scores, patients with fit or high-risk disease should receive either Isa- or D-VRd or the corresponding lite regimens, while frail patients should receive DR. The role of CAR T-cell therapies, bispecific antibodies as well as MRD-guided treatment decisions are yet to be established.
- Facon T, et al. N Engl J Med. 2019;380(22):2104-2115.
- Manier S. Treatment algorithm in transplant-ineligible patients. Session IV: NDMM - transplant-ineligible patients. EMN 2024, 18–20 April, Turin, Italy.
- Facon T, et al. Leukemia. 2022;36(4):1066-1077.
- Manier S, et al. Blood. 140(Supplement 1):1369–1370.
Medical writing support was provided by Mihai Surducan, PhD.
Copyright ©2024 Medicom Medical Publishers
Posted on
Previous Article
« Treatment should be tailored to frailty status in patients with transplant-ineligible newly diagnosed multiple myeloma Next Article
Is MRD testing ready for prime time in multiple myeloma? »
« Treatment should be tailored to frailty status in patients with transplant-ineligible newly diagnosed multiple myeloma Next Article
Is MRD testing ready for prime time in multiple myeloma? »
Related Articles
February 6, 2024
Novel standard-of-care in newly diagnosed MM
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

