https://doi.org/10.55788/79f84743
In fit patients with advanced CLL of favourable genetic risk, chemoimmunotherapy with fludarabine/cyclophosphamide/rituximab (FCR) or bendamustine/rituximab (BR) is still standard first-line treatment. In less fit patients, venetoclax/obinutuzumab (VG) is superior to chlorambucil/obinutuzumab concerning PFS [1]. Triple combinations including BTK inhibitors have shown promising results in phase 2 trials [2]. Data comparing VG with FCR or BR, nor data comparing VG plus ibrutinib (GIV) with FCR or BR as a first-line treatment in fit patients with CLL is currently available. Therefore, the 4-arm, phase 3 GAIA/CLL13 study (NCT02950051) evaluated the efficacy and safety of 3 time-limited, venetoclax-based, first-line regimens in comparison with chemoimmunotherapy in fit patients with CLL.
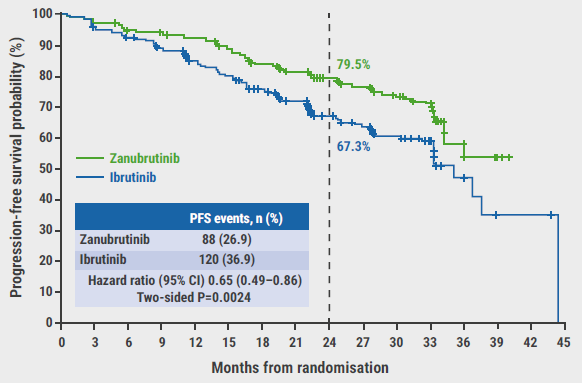
Patients (n=920) were randomised 1:1:1:1 to receive 6 cycles of FCR (for patients <65 years) or BR (>65 years), 12 cycles rituximab/venetoclax (RV), 12 cycles VG, or 12 cycles GIV. The first co-primary endpoint, a superior undetectable minimal residual disease (MRD) rate in both the VG arm and GIV arm over the FCR/BR arm at month 15, was already met in 2021 [3]. Now, Prof. Barbara Eichhorst (University Hospital Cologne, Germany) presented results on the second co-primary endpoint of the trial: interim PFS in the GIV arm versus the FCR/BR arm.
Results demonstrated superior PFS for GIV compared with FCR/BR (90.5% vs 75.5% at 3 years; HR 0.32; P<0.000001). Superior PFS was also seen in the VG arm versus FCR/BR (87% vs 75.5% at 3 years; HR 0.42; P<0.0001). PFS was not significantly different between the RV and FCR/BR arms (80.8% vs 75.5% at 3 years; HR 0.79; P=0.183). In all study arms, 3-year PFS rates were higher for patients with mutated IGHV compared with patients with wildtype IGVH. With respect to time to next treatment, GIV was superior to FCR/BR: at 3 years, 98.3% of GIV patients, 94.1% of VG patients, 92.9% of RV patients, and 87.2% of FCR/BR patients were without new treatment. Overall response data are not yet mature.
“These results demonstrate that time-limited treatment with GIV or VG improves both undetectable MRD rate at 15 months and PFS compared with standard chemoimmunotherapy in fit, previously untreated patients with CLL,” summarised Prof. Eichhorst.
- Al Sawaf O, et al. Lancet Oncol. 2020;21:1188–1200.
- Huber H, et al. Blood. 2022;139:1318–1329.
- Eichhorst B, et al. Abstract 71. ASH 2021 Annual Meeting, Atlanta, GA, USA, 11–14 December.
- Eichhorst B, et al. Time-limited venetoclax-obinutuzumab +/- ibrutinib is superior to chemoimmunotherapy in frontline chronic lymphocytic leukemia (CLL): PFS co-primary endpoint of the randomized phase 3 GAIA/CLL13 trial. Abstract LB2365. EHA2022 Hybrid Congress, 09–12 June.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Axi-cel superior to standard-of-care in older patients with relapsed/refractory large B-cell lymphoma Next Article
New subtypes of oncogenic deregulation in childhood T-ALL »
« Axi-cel superior to standard-of-care in older patients with relapsed/refractory large B-cell lymphoma Next Article
New subtypes of oncogenic deregulation in childhood T-ALL »
Table of Contents: EHA 2022
Featured articles
Post-transplant carfilzomib, lenalidomide, and dexamethasone outperforms post-transplant lenalidomide in multiple myeloma
AML
Pan-clonal score predicts first-line treatment response in AML
Quizartinib prolongs survival of newly diagnosed FLT3-ITD-mutated AML
No survival benefit of CPX-351 over FLAG-Ida in AML patients with adverse cytogenetics
Lymphocytic Leukaemia & Lymphoma
New subtypes of oncogenic deregulation in childhood T-ALL
Triple-therapy improves PFS in fit, previously untreated CLL
Axi-cel superior to standard-of-care in older patients with relapsed/refractory large B-cell lymphoma
Abscopal response in patients with relapsed or refractory Hodgkin lymphoma who failed on anti-PD1 treatment
DA-EPOCH-R is equally effective but less toxic compared with CODOX-M/R-IVAX in high-risk Burkitt lymphoma
Myeloma
Post-transplant carfilzomib, lenalidomide, and dexamethasone outperforms post-transplant lenalidomide in multiple myeloma
Triplet therapy plus early ASCT improves PFS in newly diagnosed multiple myeloma versus triplet therapy alone
Non-Cancerous Blood Disorders
Momelotinib induces a rapid and sustained improvement in haemoglobin levels in patients with myelofibrosis
Caplacizumab is safe and effective in patients with iTTP, also in the long term
Transfusion-dependent β-thalassaemia patients continue to benefit from luspatercept after 3 years of treatment
Single-dosed exa-cel leads to early and durable increase of foetal haemoglobin
PI3Kδ inhibitor leniolisib improves symptoms in patients with APDS/PASLI
Related Articles
February 18, 2021
CD58 aberrations limit durable responses to CD19 CAR T-cell therapy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

