Researchers found that levels of the yeast Debaryomyces hansenii are abundant and preferentially localized in incompletely healed intestinal wounds of mice and inflamed mucosal tissue of CD patients.
"Impaired wound healing can promote chronic inflammation, both of which are key features of inflammatory bowel diseases," senior author Dr. Thaddeus Stappenbeck of Cleveland Clinic Lerner Research Institute, in Ohio, said in a news release.
"The significance of our study is that we found an infectious component for Crohn's disease. Targeting this infection may be a viable approach to treat the disease or develop diet-based prevention strategies which are greatly needed as current therapies fail in about 50% of our patients," Dr. Stappenbeck said.
"We predict this microbe could be involved in other GI diseases that have hallmarks of injury to the inner lining of the gut and disruption of the microbiome," Dr. Stappenbeck added in an email to Reuters Health.
The researchers analyzed biopsied intestinal tissue from seven patients with Crohn's disease and 10 healthy controls. They detected D. hansenii in most diseased tissue samples but in only 10% of healthy samples.
In a separate group of CD patients they found elevated levels of D. hansenii in inflamed regions on the intestines compared to non-inflamed regions.
They confirmed higher levels of the yeast in mouse models of CD-like impaired wound healing and determined that D. hansenii is not broadly pro-inflammatory but rather contributes to disease by increasing the levels of chemokine ligand 5 (CCL5), a cytokine that recruits cells involved in inflammation.
"Taken together, our findings suggest that targeting CCL5 or the yeast itself may be viable therapeutic approaches to improve intestinal healing in patients with Crohn's disease who are infected with D. hansenii," Dr. Stappenbeck said in the news release.
"Our study supports that D. hansenii is safe in healthy individuals, but may be problematic in Crohn's patients. Our goal is to now understand how D. hansenii interacts with other components of the microbiome and the host immune system in Crohn's disease patients to affect its ability to infect damaged areas of the intestine," he added.
The researchers say more study is needed in larger samples and among patients of various ages and geographic locations. It also will be important to follow patients with the infection over time to determine any clinical importance with respect to disease severity, progression and response to Crohn's treatments.
Dr. Stappenbeck told Reuters Health that the best way detect the presence of D. hansenii, for now, is to "do an endoscopic biopsy of unhealed ulcers in the intestine, wash the biopsy carefully and culture for yeast, with sequencing for microbial identification. We have some markers in the serum that need additional validation."
The study was published in Science. In a perspective piece in the journal, Dr. June Round and Dr. Tyson Chiaro of the University of Utah, in Salt Lake City, note, "D. hansenii is likely not a common resident of the gut, because it was isolated from all samples obtained from individuals with IBD but from only one of 10 healthy donors."
"D. hansenii is an environmental yeast that is distinctive in its ability to tolerate high-salt and pH conditions and is often used in cheese and meat production. It is possible that the ability of D. hansenii to persist in extreme environments also allows it to survive within inflamed tissue. This suggests that certain dietary recommendations could be made for patients with IBD to prevent colonization with D. hansenii, but this would need to be established with clinical trials. Additionally, use of antibiotics in individuals with chronic intestinal disease should be evaluated more carefully," they write.
This research was funded in part by the Crohn's and Colitis Foundation and the National Institutes of Health.
SOURCE: https://bit.ly/2Nraf3i Science, online March 11, 2021.
By Megan Brooks
Posted on
Previous Article
« Nanotherapeutic penetrates blood-brain barrier, shows promise in glioblastoma Next Article
Anticoagulation tied to higher risk of brain hemorrhage in cancer patients with brain metastases »
« Nanotherapeutic penetrates blood-brain barrier, shows promise in glioblastoma Next Article
Anticoagulation tied to higher risk of brain hemorrhage in cancer patients with brain metastases »
Related Articles
April 30, 2021
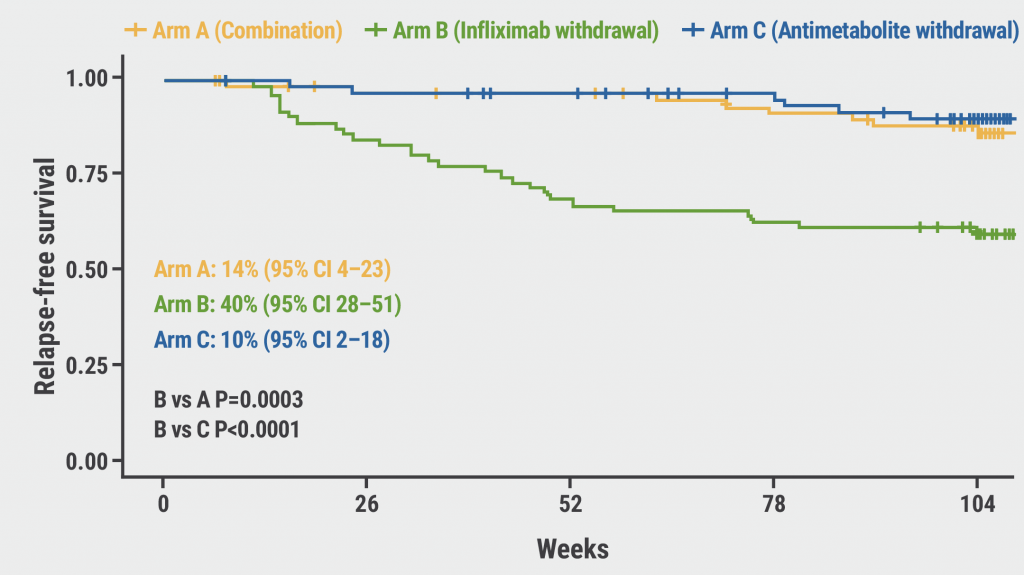
Stopping infliximab linked to relapse in ulcerative colitis
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

