"Normally, B cells mount protective antibody responses during infection as well as after vaccination," Dr. Ulrich Kalinke of TWINCORE in Hanover, Germany told Reuters Health by email. "This raises the question of whether B cell-depleted patients can profit from vaccination."
Theoretically, he said, T cells can contribute to protection against invading pathogens. However, when B cells are depleted, induction of antigen-specific T cells can be impaired.
"In particular, vaccine responses that come along with the induction of massive IFN-1 responses depend on B cells in order to effectively induce T cells," he explained. "Therefore, we propose to use vaccines in B cell-depleted patients that do not excessively induce type I IFN to induce protective T cell responses."
With regard to COVID-19, this means vector-based instead of mRNA-based vaccines. "Preclinical tests support the feasibility of this approach, whereas larger clinical studies now have to be implemented in order test the concept." Dr. Kalinke said.
As reported in Annals of the Rheumatic Diseases, the team studied T cell expansion in rituximab-treated rheumatoid arthritis (RA) patients and B cell-deficient mice after vaccination or infection with different vaccines or pathogens.
Compared to controls without RA, rituximab-treated RA patients vaccinated with the influenza vaccine Influvac had reduced expansion of influenza-specific CD8+ T cells. A similar response was seen in B cell-deficient compared to wild-type mice.
Direct IFN-1 receptor signaling of B cells was required to induce several chemokines in B cells and to support T cell help by enhancing the expression of MHC-I. When B cells were deficient, a robust immune response could not be mounted.
As an example, the authors point to a patient with granulomatosis and polyangiitis on rituximab who received a COVID-19 vaccination without regard to the rituximab treatment cycle. An analysis four weeks after the second BNT162b2 (an mRNA vaccine) dose showed that - in contrast to controls, who mounted high anti-SARS-CoV-2 IgG responses - no antibody titer was detected in the serum of this patient.
The authors conclude, "Depending on the stimulus, B cells can modulate CD8+ T cell responses. Thus, B cell depletion causes a deficiency of de novo antibody responses and affects the efficacy of cellular response including cytotoxic T cells. The choice of the appropriate vaccine to vaccinate B cell-depleted patients has to be re-evaluated in order to efficiently induce protective CD8+ T cell responses."
Dr. Asha Shajahan, Medical Director of Community Health for Beaumont Hospital in Grosse Pointe, Michigan, commented in an email to Reuters Health, "With COVID-19 being such a threat to those with immune disorders, it's important that those who are B cell-depleted have an extensive conversation with their personal immunology specialist regarding their specific scenario for vaccination."
"Many patients could be safely vaccinated and reap the benefits of vaccination after specific treatments or waiting between treatments for B cells to repopulate," she said. "Any immune response is better than none."
SOURCE: https://bit.ly/3kPfHel Annals of the Rheumatic Diseases, online July 5, 2021
By Marilynn Larkin
Posted on
Previous Article
« Even low lead levels in drinking water tied to worse kidney disease outcomes Next Article
Success rates for coronary re-access after TAVR higher in patients with short stent-frame prostheses »
« Even low lead levels in drinking water tied to worse kidney disease outcomes Next Article
Success rates for coronary re-access after TAVR higher in patients with short stent-frame prostheses »
Related Articles
September 13, 2021
Genetically engineered cells deliver RA drug in mouse study
September 4, 2019
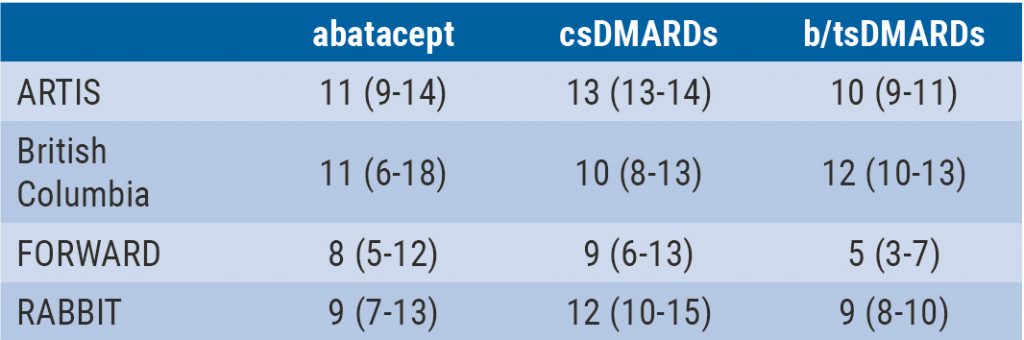
Integrated 10-year analysis confirms safety profile abatacept
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

