About a quarter of fractures happen in men, yet men are often overlooked "because it's misconstrued as a disease that mainly, if not only, affects Caucasian women," Dr. Jeffrey Curtis of the University of Alabama at Birmingham said at a November 7 press briefing at ACR Convergence, the 2020 virtual annual meeting of the American College of Rheumatology.
Dr. Curtis and colleagues reviewed the records of 9,876 male, mostly white, Medicare beneficiaries age 65 and older with an osteoporosis-related fracture between 2010 and 2014. The spine, hip and ankle were the most common sites of the fracture.
Dr. Curtis reported that 92% of these men did not have any diagnosis or treatment of osteoporosis prior to their fracture. Fewer than 6% of men had a bone-mineral density (BMD) test with dual energy x-ray absorptiometry (DXA) in the two years before their fracture.
About 3% of the men had been diagnosed with osteoporosis, but they weren't receiving any bone protective therapy. "About 2% were treated but not diagnosed - probably a slightly better option than the reverse - and only 2% of men were both diagnosed with osteoporosis and treated prior to the fracture," Dr. Curtis said.
The data also revealed a general trend for a decline in BMD testing over time; "so the under-utilization of screening with DXA testing was actually getting a bit worse, not better over time," he said.
In addition to "massive" under-diagnosis and under-treatment before a fragility fracture, the patterns were only "minimally" better after a fracture, Dr. Curtis noted. "Only about 10% of these men underwent BMD testing in the 12 months following fracture and only 9% were treated with an osteoporosis medication."
"Importantly, about 7% of the men in this large cohort went on to have one or more fractures in the next year," he added.
Dr. Curtis said there are multiple reasons for the under-diagnosis and -treatment of osteoporosis in older men. "Because osteoporosis is silent and people generally don't have symptoms in the absence of a fracture, they aren't coming in to doctors' offices asking to be screened with DXA testing. Even if they break bones, they may just not know enough to ask how to prevent the next fracture," he explained.
There is also a lack of consistent guidelines for osteoporosis screening in men, which is not the case in women.
"Among women, the World Health Organization, American Association of Clinical Endocrinologists, United States Preventive Services Task Force, National Osteoporosis Foundation (NOF) and the American Academy of Family Physicians all recommend screening women over 65 years of age. However, among men, these groups do not make any recommendation at all, except for the NOF which recommends that all men over 70, and those between the ages of 50 to 69 who have risk factors, must be screened," Dr. Curtis said in a news release.
The study had no specific funding. Dr. Curtis disclosed relationships with several makers of osteoporosis drugs.
By Megan Brooks
SOURCE: https://bit.ly/3lmHCje ACR Convergence 2020, presented November 7, 2020
Posted on
Previous Article
« Upadacitinib safety similar to other JAK inhibitors for rheumatoid arthritis Next Article
Pembrolizumab prolongs overall survival in some with advanced esophageal cancer »
« Upadacitinib safety similar to other JAK inhibitors for rheumatoid arthritis Next Article
Pembrolizumab prolongs overall survival in some with advanced esophageal cancer »
Related Articles
January 18, 2021
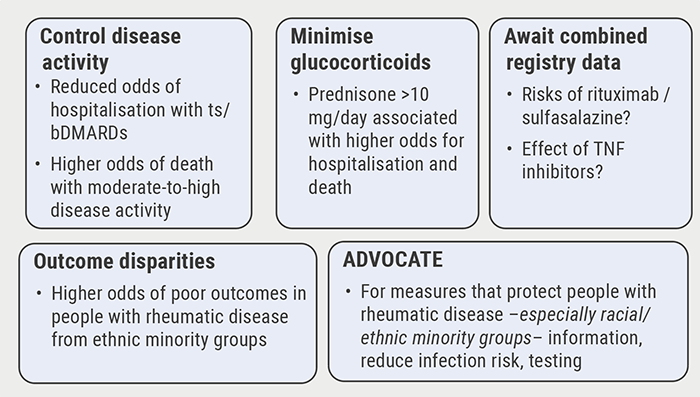
Poor disease control: a risk factor for severe COVID-19
January 18, 2021
Inflammatory disease as a risk factor for fractures
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

