Researchers examined survey data from 2,981 male residents of counties in Appalachia with elevated pneumoconiosis mortality. Overall, 20% of the men reported a rheumatoid arthritis diagnosis and 37% said they had an arthritis diagnosis, excluding rheumatoid arthritis.
A total of 11% of the men had rheumatoid arthritis treated with glucocorticoids and 4% had rheumatoid arthritis treated by disease modifying antirheumatic drugs (DMARDs).
The study included 590 men (20%) with any exposure to coal mining, and this group had a median exposure of 18 years. In addition, 821 men (28%) had silica exposure that wasn't from coal mining.
Men with exposure to coal mining were significantly more likely than those without exposure to report a rheumatoid arthritis diagnosis (odds ratio 3.5), as were men with silica exposure from something other than coal mining (OR 3.2), the study found.
This suggests that silica may explain a large part of the connection between coal mining exposure and rheumatoid arthritis, said senior study author Dr. Paul Blanc, a professor of medicine at the University of California San Francisco.
"Silica exposure occurs in mining - coal and other types - but also in many other jobs, including sandblasting," Dr. Blanc said by email. "In coal mining, coal dust likely has its own role, and may magnify silica effects."
Smoking also played a role. The study included 1,297 men (44%) who never smoked, as well as 1,226 (41%) former smokers and 458 (15%) current smokers.
Compared to never smokers, those who were current smokers or who had quit within the past three years were significantly more likely to have rheumatoid arthritis (OR 1.7), as were former smokers (OR 1.5).
Current smokers and those who had quit within the past three years were significantly more likely to have rheumatoid arthritis when they had exposure to coal mining (OR 1.6) or when then had exposure to non-coal silica (OR 3.2).
Former smokers were also significantly more likely to have rheumatoid arthritis when they had exposure to coal mining (OR 5.4) or when then had exposure to non-coal silica (OR 3.5).
One limitation of the study is that the analysis relied on self-reported information about any diagnosis of arthritis or rheumatoid arthritis, or any use of medication to treat these conditions, the study team notes in Occupational & Environmental Medicine.
The researchers also lacked workplace-specific data, making it impossible to assess in granular detail the impact of specific occupational conditions on rheumatoid arthritis risk.
Even so, the results suggest that clinicians need to be diligent about asking patients about their work history and be aware of the rheumatoid arthritis risk associated with current or former exposure to coal mining or silica, the authors write.
"Ask your patient what she or he does for a living - now and in the past," Dr. Blanc advised.
SOURCE: https://bit.ly/3GvkF7f Occupational & Environmental Medicine, online January 5, 2022.
By Lisa Rapaport
Posted on
Previous Article
« ASCO GI 2022 Highlights Podcast Next Article
CECR2 protein pinpointed as driver of breast cancer metastases »
« ASCO GI 2022 Highlights Podcast Next Article
CECR2 protein pinpointed as driver of breast cancer metastases »
Related Articles
September 4, 2019
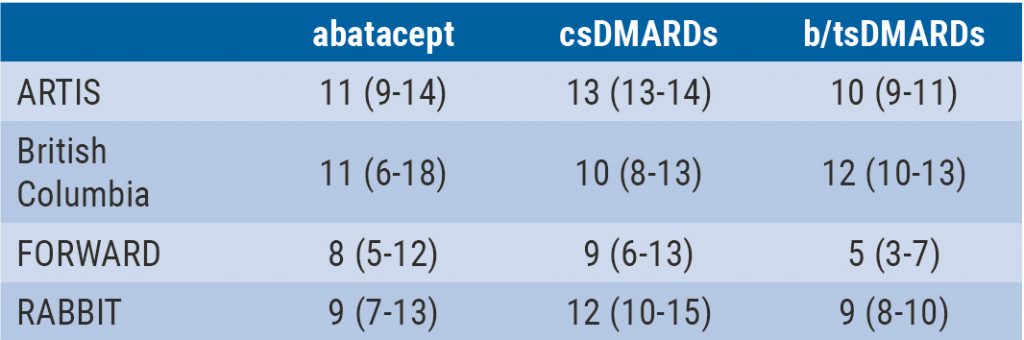
Integrated 10-year analysis confirms safety profile abatacept
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

