https://doi.org/10.55788/0479bebf
Mucus plugging is a common disease characteristic in patients with asthma and is associated with eosinophilic airway inflammation and airway obstruction [1]. “However, the effect of biologic treatment on mucus plugs in patients with severe asthma had not been assessed until the execution of the phase 2 CASCADE study (NCT03688074),” said Prof. Christopher Brightling (University of Leicester, UK). This trial randomised 116 patients with uncontrolled, moderate-to-severe asthma 1:1 to tezepelumab or placebo. The primary analysis of CASCADE demonstrated a reduced submucosal eosinophil count for patients receiving tezepelumab compared with those receiving placebo [2]. The current, exploratory, post-hoc analysis examined mucus plugging before and after treatment using CT imaging [3]. In total, 82 patients had CT scans at baseline and at the end of treatment.
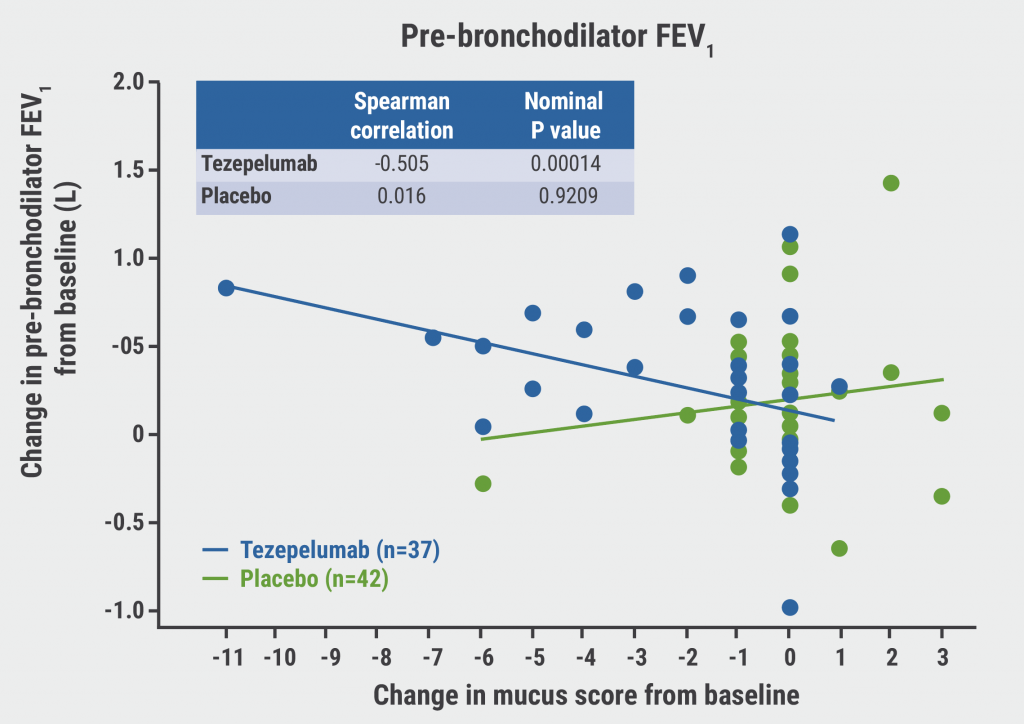
Baseline mucus scores were similar to those of comparable populations in previously published studies [1]. At baseline, blood eosinophil count was positively correlated with mucus score (ρ=0.24; nominal P=0.0006). In addition, pre-bronchodilator forced expiratory volume in 1 second (FEV1) scores were negatively related with mucus score (ρ=-0.325; nominal P=0.0017). After treatment, mucus scores were reduced in participants receiving tezepelumab but not in participants receiving placebo (mean change -1.7 vs 0.0; P=0.0007). Interestingly, post-treatment reductions in mucus scores correlated with improvements in lung function: change in pre-bronchodilator FEV1 (ρ=-0.505; nominal P=0.00014; see Figure) and pre-bronchodilator forced expiratory flow (FEF) at 25–75% (ρ=-0.535; nominal P=0.0006).
Figure: Change from baseline in lung function parameters correlates with change from baseline in mucus score [3]
“This is the first, randomised-controlled trial to demonstrate the beneficial effect of a biologic agent on mucus plugging in patients with uncontrolled, moderate-to-severe asthma,” concluded Prof. Brightling.
- Dunican EM, et al. J Clin Invest. 2018;128(3):997–1009.
- Diver S, et al. Lancet Respir Med. 2021;9:1299–1312.
- Nordenmark L, et al. Tezepelumab reduces mucus plugging in patients with uncontrolled, moderate-to-severe asthma: the phase 2 CASCADE studyALERT 4, RCT4445, ERS International Congress 2022, Barcelona, Spain, 4–6 September.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Digital asthma intervention improves health and reduces costs Next Article
Encouraging results of nintedanib in children with fibrosing ILD »
« Digital asthma intervention improves health and reduces costs Next Article
Encouraging results of nintedanib in children with fibrosing ILD »
Table of Contents: ERS 2022
Featured articles
Letter from the Editor
COVID-19: What Is New?
Does vilobelimab reduce mortality in severe COVID-19?
Awake proning not positive in COVID-19
Favipiravir may help patients over 60 years with COVID-19 to recover
Inhaled agent under investigation for COVID-19
Accurate voice-based COVID-19 diagnostic test in development
Novel scoring tool for post-COVID syndrome aids clinicians and researchers
COPD: Therapies and Innovations
Icenticaftor achieves results on top of triple inhalation therapy in COPD
STARR2: A new approach for treating COPD exacerbations
COPD medication not effective in symptomatic smokers with preserved spirometry
Do digital tools improve physical activity in COPD?
Hyperpolarised gas MRI ready for clinical use
All About Asthma
Tezepelumab in asthma: mucus plugging down, lung function up
Digital asthma intervention improves health and reduces costs
Digitally enhanced therapy lowers treatment burden and costs in severe asthma
Mepolizumab beneficial for patients with severe eosinophilic asthma
Progress in Paediatrics
Antibiotics cause increased risk of wheezing in severe RSV bronchiolitis
Inhaled corticosteroids useful in preterms with decreased lung function
Fish oil or vitamin D during pregnancy can prevent croup
Encouraging results of nintedanib in children with fibrosing ILD
Focus on Interventional Pulmonology
Head-to-head: lung volume reduction surgery vs endobronchial valves
Durable effect of endobronchial valves in severe emphysema
Cone beam CT-guided ENB improves detection of pulmonary nodules
Confirmatory mediastinoscopy not needed in resectable NSCLC
Sleep and Breathing Disorders
In the spotlight: Cancer trends in obstructive sleep apnoea
Impact of CPAP on cardiac endpoints in OSA
Sustained hypoxaemia predicts unprovoked VTE in OSA
CPAP therapy in the prevention of cardiovascular risk in patients with OSA
Other Remarkable Research
Excellent results for high-flow nasal cannula oxygen therapy in acute respiratory failure
Antifibrotic therapy may slow down FVC decline in RAILD
Intravenous N-acetylcysteine performs well in hospitalised patients
Men and women respond differently to diesel exhaust
New trends in cystic lung diseases
Related Articles

November 20, 2023
Can radiotracers predict response to PD-L1 inhibitors in early NSCLC?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

