Frailty is a biological syndrome characterised by a decreased physiological reserve for several stressors, which has been associated with a higher risk of adverse health outcomes. However, the evaluation of frailty in the setting of an acute exacerbation of ILD has not been evaluated until now [2,3]. Yet, identifying frail patients admitted with an ILD exacerbation may help with decision-making in this difficult-to-treat population.
Thus, Dr Karan Chohan (University of Toronto, Canada) and his team set out to explore the prevalence of frailty in admitted ILD patients with acute exacerbations and evaluate its association with length of hospital stay and post-exacerbation 1-year outcomes. The authors hypothesised that frail patients would have a higher likelihood for re-exacerbation and a reduced 1-year transplant-free survival. This retrospective, single-centre cohort study included 106 adult ILD patients admitted to Toronto General Hospital with an ILD exacerbation. ILD patients admitted for other reasons, such as a lung transplant assessment, were not included. At the time of hospital admission, frailty was assessed using a standardised frailty score with an index of ≥0.25 characterising frailty.
Frailty was prevalent and observed in about 40% of acute exacerbations of ILD patients. ILD patients characterised as frail were more likely to have a non-idiopathic pulmonary fibrosis diagnosis, a greater number of comorbidities (assessed in the Charlson Comorbidity Index), and a lower exercise capacity in the 6-minute walking test.
Frail ILD patients had a significantly longer hospital stay (frail vs not frail 3.2 days; 95% CI 0.6-5.4; P=0.03). They were also less likely to be transplanted compared with ILD patients without frailty (see Table). Interestingly, exacerbation rates or all-cause 1-year mortality was not significantly higher compared with ILD patients without frailty.
Table: Post exacerbation 1-year outcomes [1]
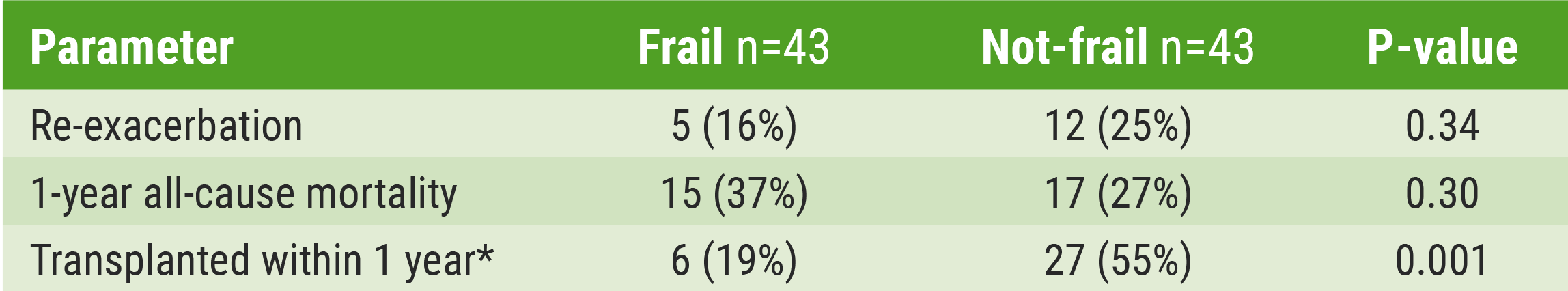
*Transplanted (frail vs not-frail): OR 0.15; 95% CI 0.04-0.51; P=0.002, adjusted for age, sex and ILD type.
- Chohan K, et al. Clinical Implications of Frailty in Acute Exacerbations of Interstitial Lung Disease. Poster P610. ATS 2020 Virtual, 5-10 Aug.
- Kolb M, et al. Eur Resp J 2018;27:180071.
- Milne KM, et al. Respirology 2017:22:728-734.
Posted on
Previous Article
« Lung cancer screening: Most patients not eligible 1-2 years prior to diagnosis Next Article
Reduced lung function associated with cognitive decline in the elderly »
« Lung cancer screening: Most patients not eligible 1-2 years prior to diagnosis Next Article
Reduced lung function associated with cognitive decline in the elderly »
Table of Contents: ERS 2020
Featured articles
COVID-19 and the Lung
COVID-19 infections: Bronchoscopy provides additional diagnostic certainty
COVID-19 vaccines: An ongoing race
COVID-19: What is the risk of reinfection?
COVID-19 App: The Dutch experience
Secondary pulmonary fibrosis: a possible long-term effect of severe COVID-19
COVID-19 survivors benefit from structured follow-up
Early pulmonary rehabilitation post-COVID-19 aids recovery
Asthma – What's New
Mild asthma: A fundamental change in management
Dupilumab shows long-term efficacy in asthma patients
Severe asthma: Oral corticosteroids maintenance therapy associated with toxicity
First-in-class tyrosine kinase inhibitor shows promise in severe asthma
Predicting individual effectiveness of biologics in severe asthma
IL-5 antagonist showed efficacy in chronic rhinosinusitis with nasal polyps
Treatment according to genotype: The future of asthma therapy?
COPD – The Beat Goes On
The role of chronic symptoms as early biomarkers of COPD development
Urgent call for studies in COPD patients aged 40-60 years
Nasal high-flow therapy: a novel treatment option for hypercapnic COPD patients
Exacerbation history is a reliable predictor of future exacerbations
Singing training effective as physical rehabilitation in COPD
Current prediction tools underestimate exacerbation risk of severe COPD patients
Exercise and Sleep: From Impaired Function to New Therapeutic Strategies
CPAP withdrawal has negative consequences for sleep apnoea patients
Physical activity improves AHI in sleep apnoea patients
The Tobacco Epidemic: From Vaping to Cannabis
Poly-use of nicotine products and cannabis: a deadly combination
E-cigarettes: A source of chronic lung inflammation
Social smoking: Do not underestimate the risks
Chronic Cough – State of the Art
LEAD study shows multiple phenotypes in many chronic cough patients
First-in-class P2X3 receptor antagonist shows promise for chronic cough treatment
Lung Cancer Detection
Lung cancer screening: Most patients not eligible 1-2 years prior to diagnosis
Distinct changes in lung microbiome precede clinical diagnosis of lung cancer
Best of Posters
Smartphone-based cough detection helpful in predicting asthma deterioration
Reduced lung function associated with cognitive decline in the elderly
Longer hospital stay and fewer transplants for frail ILD patients
Related Articles

November 9, 2021
Letter from the Editor
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

