https://doi.org/10.55788/5ead497b
In the pathophysiology of cluster headache, the hypothalamus, calcitonin gene-related peptide (CGRP), and possibly neuroinflammation are involved. “Evidence on its molecular basis is still limited,” said Dr Bendik S. Winsvold (Oslo University Hospital, Norway). Investigating cluster headache is challenging due to its low prevalence (1–1.5 per 1,000 persons, compared with 140 per 1,000 for migraine). Evidence of a possible genetic basis of cluster headache is premature. “Twin studies are not suitable due to the low prevalence of cluster headache, but a clear familial aggregation has been shown previously,” explained Dr Winsvold [2]. Most genetic studies in cluster headache have evaluated individual candidate genes. Currently, only 1 GWAS for cluster headache has been performed, which suggested variants involvement of genes encoding neprilysin and the PACAP receptor [3].
Dr Winsvold presented data from 2 independent studies, both recently published in the Annals of Neurology [4,5]. These studies were the basis of the International Consortium for Cluster Headache Genetics (CCG, www.clusterheadachegenetics.org). Therein, 2 parallel GWAS of cluster headache were conducted based on:
- 984 cluster headache cases and 3,257 controls from the Netherlands and Norway; and
- 1,443 cluster headache cases and 6,748 controls from Sweden and the United Kingdom [1].
“The 2 studies are strikingly concordant,” Dr Winsvold found. “In fact, they identified the same 4 genetic risk loci (P<5 x 10-8)”:
- on chromosome 1 near the gene DUSP10;
- on chromosome 2 near MERTK;
- on chromosome 2 near SATB2; and
- on chromosome 6 near FHL5.
Based on both studies, a meta-analysis was conducted, which found 3 additional loci:
- on chromosome 7 near ASZ1;
- on chromosome 10 near PLC1; and
- on chromosome 19 near KIR3DX1.
This concordance implies that these are true causal genetic risk factors for cluster headache, according to Dr Winsvold. The effect sizes were larger than what is usually observed in GWAS in complex disorders. “Usually, odds ratios are 1.1 or 1.2, here they are ~1.5 (range 1.30–1.61). This could suggest that cluster headache is genetically driven by a handful of high-impact variants,” explained Dr Winsvold.
The main purpose of GWAS is to understand the pathophysiology. “These first studies are not adequately powered for this purpose,” Dr Winsvold acknowledged, “but we still gained some preliminary insight. For example, one of the loci (FHL5) is a well-known risk locus for migraine. This suggests that cluster headache and migraine have a partly shared and a partly distinct genetic and molecular basis.”
- Winsvold BS, et al. International Consortium for Cluster Headache Genetics: two initiatives report first genome-wide association hits. AL070, IHC 2021, 8–12 September.
- O'Connor E, et al. J Headache Pain. 2020;21(1):37.
- Bacchelli E, et al. J Headache Pain. 2016;17(1):114.
- Harder AVE, et al. Ann Neurol. 2021;90(2):203–16.
- O'Connor E, et al. Ann Neurol. 2021;90:193–202.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Functional brainstem somatotopy of the trigeminal nerve during nociception Next Article
Largest genome-wide association study of migraine to date »
« Functional brainstem somatotopy of the trigeminal nerve during nociception Next Article
Largest genome-wide association study of migraine to date »
Table of Contents: IHC 2021
Featured articles
Letter from the Editor
COVID-19
Telemedicine beneficial for headache care during the pandemic
Comparison of headaches after SARS-CoV-2 vaccination
Grey matter cortical changes in patients with persistent headache after COVID-19
Increased risk of cerebral venous thrombosis in COVID-19
Patient Perception and Symptoms
Predictors of health-related quality of life in cluster headache
Dry eye disease is more prevalent in migraine
Voice change and throat swelling are cranial autonomic symptoms in primary headache
Association between physical inactivity and headache disorders
Increased suicidal attempts and risks of ideation in medication-overuse headache
Cardioembolic Comorbidities
AI-enabled ECG algorithm predicts atrial fibrillation risk in migraine
Migraine may not be a risk factor for stroke
Imaging
Functional brainstem somatotopy of the trigeminal nerve during nociception
Morphological changes in cluster headache between attacks
Interictal pontine metabolism in migraine patients without aura
Genome-Wide Association Studies
Largest genome-wide association study of migraine to date
Robust evidence that cluster headache has a genetic basis
Pharmacological Treatment
Insights in drug-drug interactions facilitate rational polypharmacy
Rimegepant confers long-term improvements in MMDs
First real-world effectiveness data of erenumab is promising
Galcanezumab effective in patients with episodic or chronic cluster headache
Central effects and affected somatosensory processing with galcanezumab in migraine
Long-term safety and tolerability of atogepant in migraine
Non-Pharmacological Treatment
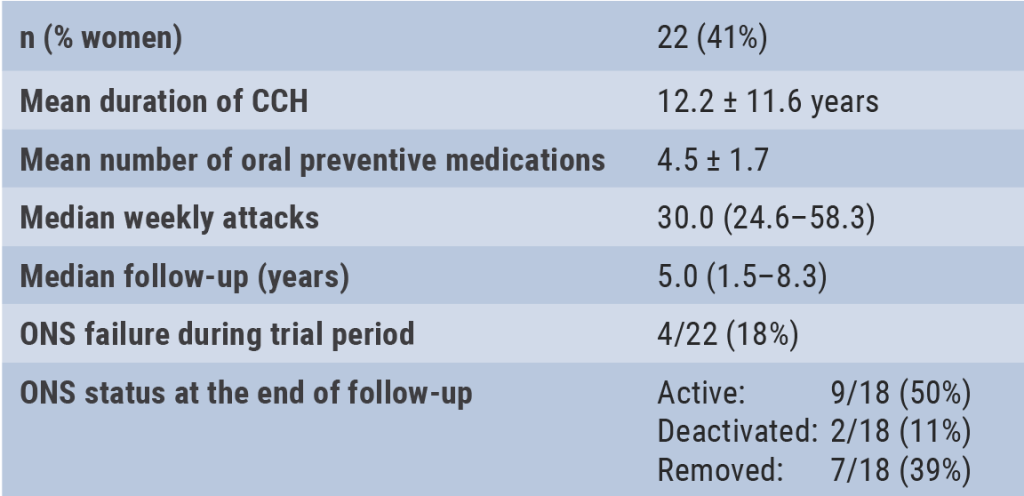
Occipital nerve stimulation effective and safe in chronic cluster headache
Related Articles
August 18, 2021
Pregnant migraine patients at higher risk of complications
June 16, 2021
Efficacy and safety of eptinezumab in acute migraine
August 18, 2021
Occipital nerve stimulation in drug-resistant cluster headache
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

