Based on 182 patients with chronic or episodic migraine who were randomly assigned for four months to diets designed to manipulate omega-3 and omega-6 fatty acids, researchers found that boosting omega-3s while also lowering omega-6s led to a reduction of 1.7 headache hours per day and a decrease of four headache days per month, according to results published in The BMJ.
"This is the first moderate-sized controlled trial showing that targeted changes in diet can decrease physical pain," said the study's lead author, Dr. Christopher Ramsden, a clinical investigator at the National Institute on Aging in Baltimore. "The biochemical findings support the biological plausibility of this type of approach."
"There is an unmet need for safe and effective treatments for chronic pain," Dr. Ramsden said in an email. "The magnitude of pain reduction (about 30-40% compared to control diet) seen in this trial was similar to that provided by pain medications. The findings could open the door to new approaches for managing pain in humans, but we still know very little. With additional study, it may ultimately be possible to design better diets and integrate targeted dietary changes alongside medications to improve the lives of patients with chronic pain."
Previous studies in humans and animal models have linked dietary fatty acids to pain, Dr. Ramsden said.
"Diets alter the amounts of omega-3 and omega-6 fatty acids in the nervous system and other tissues linked to chronic pain," he added. "These fatty acids are converted by the body into biochemical mediators of pain."
The researchers say they chose to look at omega-3 fatty acids because these compounds are precursors to hydroxydocosahexenoic acid (17-HDHA), the precursor for several families of oxylipins reported to have potent antinociceptive effects in experimental models, and has been linked to lower pain scores in patients with arthritis. Omega-6 fatty acids, in contrast, are linked with exacerbation of pain and inflammation.
To explore whether diets rich in omega-3 fatty acids would increase circulating levels of 17-HDHA and influence the frequency and severity of headaches, Dr. Ramsden and his colleagues ran a clinical trial at the University of North Carolina in 2018-2019.
Among the 182 recruited patients, of whom 88% were female, baseline mean HIT-6 score was 62.7 (scale ranges from 36 to 78 points), indicating a severe impact of headaches on quality of life, the authors note. At study entry, participants averaged 16.3 headache days per month and 5.4 headache hours per day, and used an average 4.3 headache-related drugs per person.
Study participants were randomly assigned to one of three diets for 16 weeks. The control diet included typical levels of omega-3 fatty acids (EPA and DHA) at less than 150 mg/day, and omega 6 (linoleic acid) at around 7% of energy. One intervention diet, H3, increased EPA and DHA to 1.5 g/day and maintained linoleic acid at around 7% of energy while the other diet, H3+H6, increased EPA and DHA to 1.5 g/day and decreased linoleic acid to 1.8% of energy or less.
Participants received regular dietary counseling and access to online support information during the study, and they all filled out the headache impact test (HIT-6), a six-item questionnaire assessing the impact of headaches on their lives. Headache frequency was documented in electronic diaries.
Over 16 weeks, both interventional diets led to an increase in circulating 17-HDHA levels compared to the control diet. While HIT-6 scores improved in both intervention groups, the difference from the control group wasn't statistically significant. Still, headache frequency decreased significantly in both intervention-diet groups. The H3+H6 diet group saw a reduction of 1.7 headache hours per day and four headache days per month. The H3 diet group saw smaller improvements, with a reduction of 1.3 headache hours per day and two headache days per month.
The new study suggests that diet does play a role in migraine and "therefore dietary alterations can aid in treatment," said headache specialist Dr. Lauren Natbony, an assistant professor of medicine at the Icahn School of Medicine at Mount Sinai in New York City.
"This study specifically looks at dietary intake of omegas and their impact on migraine," Dr. Natbony said in an email. "It shows that a high omega-3 diet (and low omega-6 diet) can decrease the frequency and severity of headache. It can also reduce the number of acute medications needed to treat a headache attack."
The headache reductions seen in the study "are comparable to many medication trials including botulinum toxin A and CGRP monoclonal antibodies," Dr. Natbony said. "It is also important to note that a reduction was seen in chronic migraine, which is a notoriously difficult condition to treat."
While the researchers did not see a statistically significant improvement in HIT-6 scores, "there was a robust reduction in headache frequency and severity that cannot be ignored. The HIT-6 test is only one metric to determine improvement and is a subjective evaluation of the impact of headache on quality of life."
"My takeaway as a clinician is that a high omega-3/low omega-6 diet may be a good adjunct treatment in those patients with migraine already on prescription medication," Dr. Natbony said. "It may also be a good therapy in those who do not tolerate or who have contraindications to pharmaceuticals. There have been other small studies that have shown a reduction in headache days per month with a high omega-3 diet. Thus, this study adds to the existing literature."
SOURCE: https://bit.ly/3yehSvI and https://bit.ly/2SEvkJY The BMJ, online July 1, 2021.
By Linda Carroll
Posted on
Previous Article
« Single-cell mRNA signaling facilitates diagnosis of childhood and adult kidney tumors Next Article
Obesity increases the risk of immunogenicity to adalimumab in IBD »
« Single-cell mRNA signaling facilitates diagnosis of childhood and adult kidney tumors Next Article
Obesity increases the risk of immunogenicity to adalimumab in IBD »
Related Articles
July 30, 2019
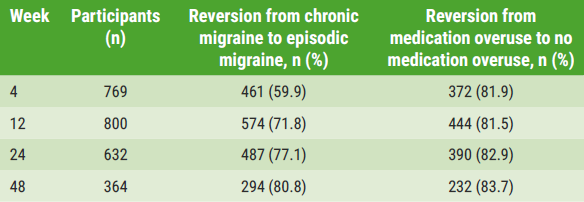
Fremanezumab efficacy and safety maintained over 1 year
October 27, 2020
Early initiation of lasmiditan improves migraine outcomes
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

