 The CAR-hematotox score predicts the risk for prolonged neutropaenia, severe infections, and poor treatment outcomes after CD19 CAR T-cell therapy [2,3]. However, the use of this tool in patients with relapsed/refractory MCL undergoing CD19 CAR T-cell therapy has not yet been established. Therefore, the international, multicentre, retrospective study headed by Dr Rejeski analyzed the applicability of the CAR-hematotox score in 103 patients with relapsed/refractory MCL receiving brexu-cel. There was an accompanying poster at ASH 2022, that used this technique as well, correlating Hematox-scores calculated prior to treatment to hematological toxicities in patients receiving BCMA-targeting CAR-T regiment with ciltacabtagene autoleucel or idecabtagene vicleucel [2].
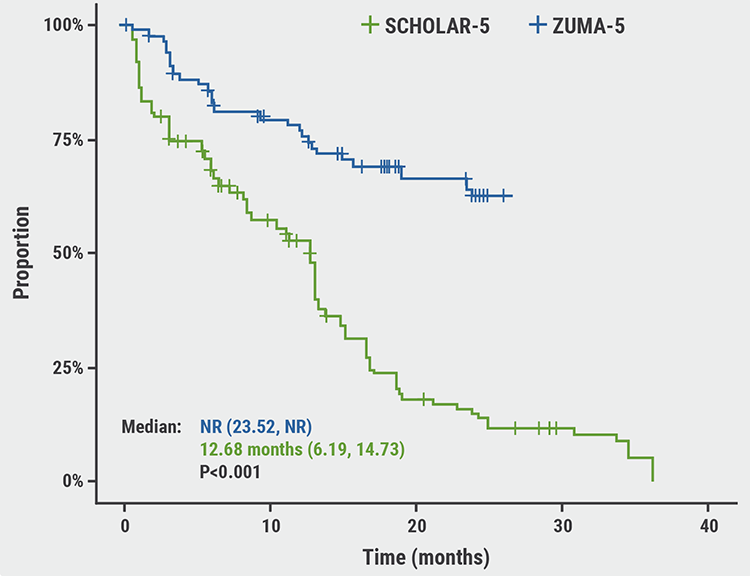
The CAR-hematotox score predicts the risk for prolonged neutropaenia, severe infections, and poor treatment outcomes after CD19 CAR T-cell therapy [2,3]. However, the use of this tool in patients with relapsed/refractory MCL undergoing CD19 CAR T-cell therapy has not yet been established. Therefore, the international, multicentre, retrospective study headed by Dr Rejeski analyzed the applicability of the CAR-hematotox score in 103 patients with relapsed/refractory MCL receiving brexu-cel. There was an accompanying poster at ASH 2022, that used this technique as well, correlating Hematox-scores calculated prior to treatment to hematological toxicities in patients receiving BCMA-targeting CAR-T regiment with ciltacabtagene autoleucel or idecabtagene vicleucel [2].At baseline, high CAR-hematotox scores (HT-high) were related to aggressive disease biology, increased bone marrow infiltration, a higher number of prior treatments, and increased disease activity. It was demonstrated that patients with HT-high prior to CAR-T therapy had higher risk for haematologic toxicity than patients with HT-low: neutropaenia (median 14 days vs 6 days; P<0.001); aplastic phenotype (47% vs 0%; P<0.001). Anaemia and profound or prolonged cytopaenia were also more frequently observed in HT-high patients. Furthermore, severe infections were more common in HT-high patients than in HT-low patients (30% vs 5%; P=0.001), mostly driven by an increase in bacterial infections (28% vs 5%; P=0.002). Finally, after 720 days of follow-up, HT-high scores were associated with poorer progression-free survival (38% vs 79%; P<0.0001) and overall survival (52% vs 90%; P=0.00016) than HT-low scores.
The authors concluded from this initial analysis that stratifying patients for the risk of haematological toxicity may aid physicians to tailor the management of their patients. Medicom spoke to Dr Rejeski, lead study investigator, about his results.
What is the unmet need that the CAR-hematotox score is trying to fill?
Dr Rejeski: We have known about different side effects of CAR T-cell therapy for a while; in particular, cytokine release storm (CRS) and neurotoxicity, also referred to as immune effector cell-associated neurotoxicity syndrome (ICANS), which are both unique toxicities following CART cell therapy, occurring in up to 67% of patients with leukaemia and 62% of patients with lymphoma [3]. Although these treatment-related adverse events were well described in initial trials, with the field moving forward into real-world evidence, we are starting to gain an appreciation for previously unknown side effects, or less well described side effects. Among those, I think haematological toxicity, meaning profound and prolonged cytopaenias, is especially relevant. These can occur long after lympho-depleting chemotherapy, or long after resolution of clinical CRS and also the concomitant infectious complications, which are a result of the combined cellular immunosuppression and humeral immunosuppression that is conferred by CD19- or BCMA-directed CAR T-cell therapy. We really sought to describe haematological toxicity, focusing on identifying predictive biomarkers of haematological toxicity, and in order to predict haematological toxicity, we developed a model we call the Car-Hemotox, score. The score is comprised of factors related to the baseline inflammatory state, eg CRP and ferritin, and also measures of baseline haematologic reserve: ANC (neutrophil count), haemoglobin, and platelet count. We found in 2 external validation courts, one from the US and one from Europe, that the score was capable of identifying high-risk candidates prior to lympho-depleting chemotherapy [4]. We then went on to identify patients who had high versus low risk for haematological toxicity and demonstrated that patients who were high risk also had a high risk of infections and poor treatment outcomes [5].We next asked the question: is this also true for patients receiving brexu-cel for relapsed/refractory mantle cell lymphoma? And in another abstract that was presented at ASH2022, we characterised the influence of the CAR-hematox score on toxicity and clinical outcomes in 102 patients receiving BCMA CAR-T with ciltacabtagene autoleucel (n=7) or idecabtagene vicleucel (n=95) in a standard-of-care setting across 5 international CAR-T centres [2]. Again, in that study, we observed that when comparing patients who had a high Hematox score (≥2) with those who had a low score (0 or 1), the patients higher Heamtox scores had a higher risk for haematological toxicity, with longer prolonged neutropaenia, 9 days or longer. On the contrary, the patients predicted to be low-risk had, in general, less than 7 days of severe neutropaenia. This translated to a significantly lower rate or incidence rates of severe infections in the low-risk patients compared with the high-risk patients. The patients with high Hematox scores had higher non-relapse mortality, with infections really driving non-relapse mortality after CAR T-cell therapy.
CRS and ICANS are regarded as these flashy new side effects of CAR T-cell therapy. But in the real world setting, patients actually die of infectious complications. So, for instance, we found that 1 out of 10 patients died within the first year from non-relapse related causes. Concerningly, of those deaths, about 75 to 80% were attributable to infectious complications. Oftentimes the infectious complications are a result of very profound sustained myelosuppression. Our data supports the notion that haematological toxicity and infectious complications are intrinsically linked. I think that this fact underlines why the Hematox score may be of relevance for identifying patients who are at high risk for non-relapse mortality. Finally, we looked at clinical outcomes and we see that there was inferior progression-free survival and overall survival in both the myeloma and the Mantle Cell lymphoma cohorts for patients the Hematox score had predicted were high risk patients.
Clinical implications?
Dr Rejeski: In summary, we think we can identify particularly poor-risk or ultra-high risk patients prior to therapy initiation using the Hematox score, and we see several clinical implications. We think that it is important for general risk stratification prior to most therapies, to understand which patients are at high risk and which are at low risk. High-risk patients, these are patients who may benefit from a specific prophylaxis regimen, such as antifungal prophylaxis, because they fit into the IDSA consensus guidelines for a mold active fungal prophylaxis. The same may be true for antibacterial prophylaxis. This targeted approach was something that we demonstrated in a multi-variate analysis in one of our published studies [5].On the other hand, identifying the low-risk patients could help us target them for antibiotics-sparing procedures. Essentially every patient (about 86%) has febrile neutropaenia In the first 10 days after CAR T-cell therapy. We know that this results in most patients being worked up for febrile neutropaenia, even though this fever syndrome is not necessarily attributable to an infectious cause. We think that the low-risk patients identified by the Hematox-score may be the patients who could be spared with antibiotics.
Collectively, these data really highlight the fact that inflammation is a really relevant factor, baseline inflammatory state is a really relevant factor in patients receiving CAR T-cell therapy because CRP and ferritin are basically hinting to us as clinicians that these patients have profound immune dysregulation, that they have inflammatory micromilieu which is not necessarily advantageous when patients receive CAR T-cell therapy.
Did you see differences in the trends in outcomes across diseases?
Dr Rejeski: Not really- we found that, at least in terms of predicting haematological toxicity- we saw consistent findings. In multiple myeloma, we actually found that the score also identified patients at higher risk for ICANS, which wasn't the case in the mantle cell lymphoma cohort.Our data essentially suggest that across disease entities, these same risk factors that we identified for large B-cell lymphoma, hold true in patients receiving CAR T-cell treatment for mantle cell lymphoma, or multiple myeloma as well. I think one of the reasons why this is the case is because these diseases, multiple myeloma, mantle cell lymphoma, are also bone marrow-derived or have a predominance of bone marrow infiltration. We think that this pathological characteristic is something that predisposes patients for haematological toxicity because of local inflammatory processes that occur when there is CAR T-cell related inflammation within the haematopoietic niche.
What's next?
Dr Rejeski: Clearly, we are interested in prospective validation of the Hematox score. First, we programmed a score calculator with the help of the German Lymphoma Alliance, which can be found online (https://www.german-lymphoma-alliance.de/Scores), to make it readily available across different centers. I'd encourage people to check that out.We are also asking whether we use the score now to really develop clinical trials , especially for those studies specifically looking at the benefit of antibiotic prophylaxis and early growth factor support. There is recent data showing that that is safe in the CAR T-cell space; I think that those are the next steps.
Lastly, I think using the score will help us to identify or understand why patients develop haematological toxicity. I think that is an unmet clinical need, that we have yet to understand pathophysiologically what is even happening in these patients who are at-risk to develop haematological toxicity.
References:
- Rejeski K, et al. The CAR-Hematotox Score Identifies Patients at High Risk for Hematological Toxicity, Infections and Poor Clinical Outcomes Following Brexucabtagene Autoleucel in Relapsed/Refractory Mantle Cell Lymphoma. Abstract 264, ASH 64th Annual Meeting, 10–13 December 2022, New Orleans, USA.
- Rejeski K. et al. The CAR-Hematotox Score As a Prognostic Model of Toxicity and Response in Patients Receiving BCMA-Directed CAR-T for Relapsed/Refractory Multiple Myeloma, Poster 3343, ASH 64th Annual Meeting, 10–13 December 2022, New Orleans, USA.
- Santomasso BD, et al. Clinical and Biological Correlates of Neurotoxicity Associated with CAR T-cell Therapy in Patients with B-cell Acute Lymphoblastic Leukemia. Cancer Discov. 2018 Aug;8(8):958-971.
- Rejeski K, et al. Blood. 2021;138(24):2499–2513.
- Rejeski K, et al. The CAR-HEMATOTOX risk-stratifies patients for severe infections and disease progression after CD19 CAR-T in R/R LBCL. J Immunother Cancer. 2022 May;10(5):e004475
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Metabolic tumor volume predicts response to loncastuximab tesirine in DLBCL Next Article
Real world outcomes show ibrutinib delays need for next treatment longer than acalabrutinib in first-line CLL »
« Metabolic tumor volume predicts response to loncastuximab tesirine in DLBCL Next Article
Real world outcomes show ibrutinib delays need for next treatment longer than acalabrutinib in first-line CLL »
Related Articles
February 4, 2022
Novel anti-CD19 plus lenalidomide prolonged survival in R/R DLBCL
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

