Prof. Sabine Eichinger (Medical University Hospital of Vienna, Austria) reviewed the discovery of VITT and discussed algorithms for VITT diagnosis and treatment [1]. The first diagnosed case of VITT was a 49-year-old woman. On 17 February 2021, she received the first COVID-19 vaccine (ChAdOx1 nCov-19, AstraZeneca) and experienced mild fever, headache, and myalgia, which resolved after 2–3 days. From day 5, she experienced increasing abdominal pain, chills, and vomiting. In the morning of day 10, the patient was admitted to a local hospital and tested negative for SARS-CoV-2. She had a low platelet count (18/mm³) and elevated D-dimer (35 µg/mL), gamma-GT (141 U/L), and CRP (8.8 mg/dL). Computer tomography (CT) imaging showed portal vein thrombosis and peripheral pulmonary embolism. The patient was transferred to a tertiary hospital in good condition. Due to high fibrinogen levels (101 mg/dL), she received 4000 IU enoxaparin subcutaneously in the evening of day 10. On day 11, she had massive abdominal pain. A repeat CT showed progression of portal vein thrombosis including splenic and upper mesenteric veins, oedema of intestinal walls due to malperfusion, and small thrombi in the infrarenal aorta and both iliac arteries. Laboratory results were similar to those of day 10. There were no safe therapeutic options due to increased bleeding risk. Low-dose unfractionated heparin was stopped after 1.5 hours due to tachycardia. The patients developed elevated lactate levels (3.6 mmol/L), haematemesis, was transferred to intensive care unit, and died on the evening of day 11. Autopsy confirmed cerebral thrombosis which was supported by clinical parameters taken prior to death.
Several differential diagnoses were considered and dismissed: COVID-19 (patient repeatedly tested negative), disseminated intravascular coagulopathy (DIC; no signs of malignancies or sepsis), antiphospholipid syndrome (aPTT normal, and anti-cardiolipin/β2-glycoprotein antibodies negative), thrombotic thrombocytopenic purpura (no haemolysis, no schistocytes, macrothrombosis), and heparin-induced thrombocytopenia (no heparin before onset of symptoms, severe DIC very unusual). The mechanisms of VITT were discussed in detail by Prof. Greinacher (see Mechanisms of COVID-19 vaccine-induced thrombotic thrombocytopenia) [2].
Platelet activation tests of 4 patients with suspected VITT finally led to the discovery of VITT [1]. Serum of suspected VITT patients was spiked with normal platelets and platelet factor 4 (PF4), which led to strong platelet activation and which was not the case with heparin or intravenous immunoglobulins (IVIG) controls [3].
Prof. Eichinger also presented patient characteristics from different research groups. While in mainland Europe most patients (n=16) were women (≥80%) and maximum 54 years old, only 57% of patients in the United Kingdom (n=23) were female and ≤77 years of age [3–5]. First reported cases from Canada (n=3) are in line with British findings: 33% female and >60 years old.
To aid in the diagnosis, the acronym VITT can be used:
- Vaccine (until now AstraZeneca and Johnson & Johnson/Janssen)
- Interval (symptoms start between 5–10 days)
- Thrombosis
- Thrombocytopenia
A diagnostic and treatment algorithm was presented and the confirmation assay PIFPA is now available (see Figure).
Figure: Diagnostic and treatment algorithm for patients with suspected VITT. Modified from [1,3]

In conclusion, the diagnosis of VITT and supporting diagnostic tools have improved over the last few months. However, typical characteristics of patients at risk and predictive factors remain unknown to date.
- Eichinger S. Vaccine induced immune thrombotic thrombocytopenia. P241-2, EHA 2021 Virtual Congress, 9–17 June.
- Greinacher A. p217-3, EHA 2021 Virtual Congress, 9–17 June.
- Greinacher A, et al. N Engl J Med 2021; 384:2092–101.
- Schulz NH, et al. N Engl J Med 2021; 384:2124–30.
- Scully M, et al. N Engl J Med 2021; 384:2202–11.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Novel targets in myelofibrosis: overview of emergent therapies Next Article
Mechanisms of COVID-19 vaccine-induced thrombotic thrombocytopenia »
« Novel targets in myelofibrosis: overview of emergent therapies Next Article
Mechanisms of COVID-19 vaccine-induced thrombotic thrombocytopenia »
Table of Contents: EHA 2021
Featured articles
Lymphoma
Immuno-oncology agents are effective in treating classic Hodgkin’s lymphoma
MATRix with ASCT: best long-term survival for primary CNS lymphoma
Naratuximab emtansine + rituximab safe and effective in diffuse large B-cell lymphoma
The journey ahead for CAR T-cell therapy in r/r follicular lymphoma
ZUMA-5 vs SCHOLAR-5: Axicabtagene ciloleucel significantly improves FL outcome
Promising chemo-free treatment options in r/r DLBCL
Leukaemia
Sabatolimab achieved durable responses in patients with high-risk MDS and AML
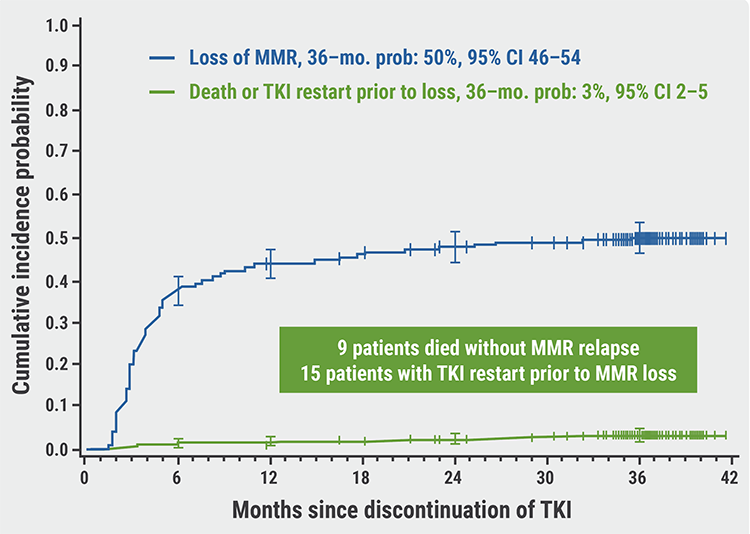
Final analysis of EURO-SKI: primary endpoints met in chronic myeloid leukaemia
Favourable outcomes with zanubrutinib versus ibrutinib in patients with r/r CLL
Oral azacitidine improves overall survival in patients with acute myeloid leukaemia
Reduced-intensity conditioning ASCT is effective in older patients with AML
ELEVATE-TN: Acalabrutinib shows long-term efficacy in chronic lymphocytic leukaemia
ELEVATE-RR: Acalabrutinib demonstrates similar efficacy and better safety versus ibrutinib
Fixed 12 cycles and MRD-guided venetoclax consolidation effective in CLL
GLOW: Ibrutinib + venetoclax showed superior PFS as first-line CLL treatment
Myeloma and Myelofibrosis
Novel targets in myelofibrosis: overview of emergent therapies
Immune therapy of multiple myeloma
MAIA results confirm superior efficacy of daratumumab with standard-of-care
ANDROMEDA: Addition of daratumumab showed superior efficacy in patients with AL amyloidosis
Thrombotic and Thrombocytopenic Disorders including COVID-19 related
Acquired TTP: new treatments and updated guidelines
Maternal screening to prevent foetal and neonatal alloimmune thrombocytopenia
Fostamatinib effectively increased platelet counts in immune thrombocytopenic purpura
Physiopathology of coagulopathy in haematological malignancies and COVID-19
Haemostatic abnormalities are associated with mortality in COVID-19
Mechanisms of COVID-19 vaccine-induced thrombotic thrombocytopenia
COVID-19 vaccine-induced immune thrombotic thrombocytopenia: discovery and diagnosis
Haemoglobinopathies
Luspatercept improved anaemia in patients with non-transfusion-dependent β-thalassaemia
Personalising treatment for sickle cell disease
Gene therapy: A promising approach for hereditary haemoglobinopathies
Related Articles
August 5, 2021
Immune therapy of multiple myeloma

August 5, 2021
Letter from the Editor
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

