As Dr. Carlos Mena told Reuters Health by email, "Our study shows a very low rate of guideline-directed medical therapy amongst the highest-risk patients when sending them for invasive procedures, at a time where clinicians are afforded an opportunity to optimize their medical risk management."
The clinical pathway for PVI offers a chance to improve patients' care and outcomes, including curbing cardiovascular events, limb loss and mortality, Dr. Mena of Yale School of Medicine, in New Haven, Connecticut, and colleagues note in the Journal of the American College of Cardiology.
The researchers defined GDMT as the composite prescription of aspirin or any other antiplatelet agent, a statin and an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blocker (ARB) if hypertension were present. Using these criteria, they examined data from 2016 to 2019 on more than 28,000 lower-extremity PVIs from 244 centers.
The magnitude of the site-level variation for GDMT prescriptions was summarized through adjusted median odds ratios (MORs) before and after the procedure. Adjustments were made for age, sex, race, insurance status, and a number of other factors including comorbidities and specific aspects of the procedure.
Before PVI, 77% received any antiplatelet therapy, 70% were on statins and 49% received ACE inhibitors/ARB. Only 36% were on all eligible GDMTs.
Following the procedure there was an absolute increase in any antiplatelet therapy to 92% and a significant increase in statins to 77%. However, there was a drop in ACE inhibitor/ARB use to 48% and use of all three GDMTs although increased remained at a suboptimal 43.0%
There were high-performing centers that attained GDMT rates close to 100%, but performance was uneven with significant site variability before (adjusted MOR,1.31) and after PVI (aMOR, 1.35).
Dr. Mena observed that "MOR, which is an indicator of the degree of variability of GDMT use across vascular centers, changed little after adjusting for patient-level factors. This means that the differences across sites for the quality of GDMT patterns, are not explained by patient characteristics, but rather, that going from one facility to another, your chances of getting GDMT may vary significantly, just by ways that a particular center, for example, may or may not have coordinated approaches to pay attention to this aspect of care."
Thus, he concluded, "Before opting to send patients with critical limb ischemia for invasive procedures, evidence-based cardiovascular medications need to be optimized in order to prevent future fatal and non-fatal cardiovascular and limb events in this vulnerable population."
Commenting on the findings by email, vascular-medicine specialist Dr. Ido Weinberg of Massachusetts General Hospital, in Boston, told Reuters Health, "As the authors point out, best practices have the potential to improve patient outcomes, including reduced mortality and improved limb outcomes. The differences in outcomes between patients who are on best medical therapy and those who are not can be staggering."
Dr. Weinberg, associate professor of medicine at Harvard Medical School, added, "There are many potential barriers to best medical therapy in patients with critical limb ischemia. In other words, fixing the problem is not as easy as it may sound. These barriers include prescriber and patient knowledge gaps. More specifically, there is much to learn about providing equitable care to various patient groups including women, persons of color and people of various socio-economic backgrounds."
"One potential way to improve medical therapies in patients with critical limb ischemia." he concluded, "is through team-work. Critical limb ischemia centers have the potential to improve patient care."
SOURCE: https://bit.ly/3euzOeP Journal of the American College of Cardiology, online March 8, 2021.
By David Douglas
Posted on
Previous Article
« Epilepsy proteome pinpoints GNB1 pathways, other new treatment targets for epilepsy Next Article
Bedside leucocyte esterase testing can help rule out septic arthritis in native joints »
« Epilepsy proteome pinpoints GNB1 pathways, other new treatment targets for epilepsy Next Article
Bedside leucocyte esterase testing can help rule out septic arthritis in native joints »
Related Articles
September 9, 2020
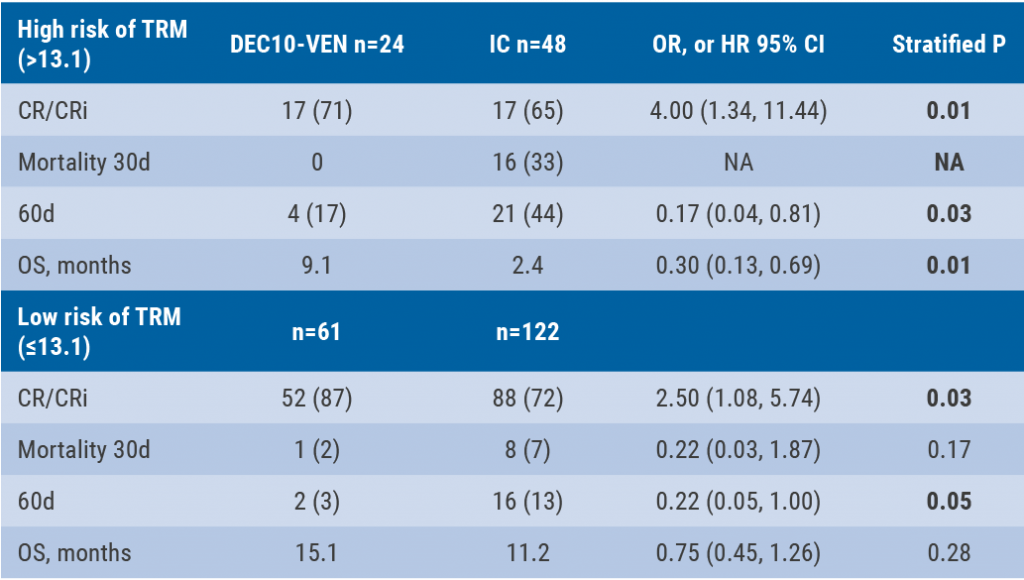
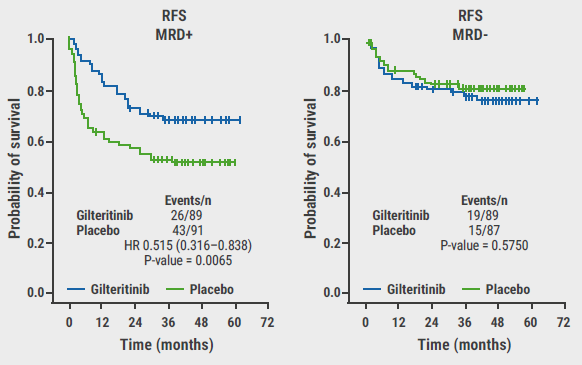
DEC10-VEN superior to intensive chemotherapy in high-risk AML
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

