https://doi.org/10.55788/1e3a56de
In patients with PNH, targeting the terminal complement pathway at C5 with ravulizumab or eculizumab helps to control intravascular haemolysis [1,2]. However, residual anaemia, mostly due to extravascular haemolysis, occurs in up to two-thirds of patients [3]. Iptacopan, a first-in-class, oral, selective factor B inhibitor, targets the complement system proximally, via the alternative pathway [4]. A recently published phase 2 study showed that iptacopan controlled haemolysis in a group of 10 patients with PNH and active haemolysis who did not respond well to eculizumab [5].
To further investigate iptacopan, the Apply-PNH trial (NCT04558918) randomised 97 patients with PNH and residual anaemia despite treatment with standard-of-care 8:5 to iptacopan 200 mg oral, twice daily or to the intravenous anti-C5 standard-of-care they received before randomisation [6]. The primary endpoints were:
- Achieving an increase from baseline in haemoglobin of ≥2 g/dL in the absence of red-blood cell transfusions
- Achieving an increase from baseline in haemoglobin of ≥12 g/dL in the absence of red-blood cell transfusions.
Prof. Régis de Latour (Saint-Louis Hospital, France) presented the primary results after 24 weeks of treatment.
In total, 51 out of 60 patients in the iptacopan arm achieved the first primary endpoint compared with 0 out of 35 in the standard-of-care arm, with a population estimate difference of 80.3% (95% CI 71.3–87.6; P<0.0001). The second primary endpoint was reached by 42 patients in the iptacopan arm and by 0 patients in the standard-of-care arm. The corresponding population estimate difference was 67.0% (95% CI 56.3–76.9; P<0.0001). Furthermore, transfusion could be avoided in 60 out of 62 patients in the iptacopan arm and in 14 out of 35 patients in the standard-of-care arm (population estimate difference 70.3%; 95% CI 52.6–84.9; P<0.0001).
The safety analysis showed an apparent higher incidence of headache (16.1% vs 2.9%) and diarrhoea (14.5% vs 5.7%) in the iptacopan arm, but breakthrough haemolysis was more common in the standard-of-care arm than in the iptacopan arm (17.1% vs 3.2%). Finally, the rate of serious treatment-emergent adverse events seemed to be higher in the standard-of-care arm (14.3% vs 9.7%).
“Iptacopan may represent a practice-changing, oral, outpatient therapy for patients with PNH who do not respond well to ravulizumab or eculizumab,” suggested Prof. de Latour.
- Hillmen P, et al. N Engl J Med. 2006;355:1233–1243.
- Kulesakararaj AG, et al. Blood. 2019;133(6):540–549.
- Risitano AM, et al. Front Immunol. 2019;10:1157.
- Schubart A, et al. Proc Natl Acad Sci USA. 2019;116:7926–7931.
- Risitano AM, et al. Lancet Haematol. 2021;8(5):e344–e354.
- de Latour RP, et al. Oral Monotherapy with Iptacopan, a Proximal Complement Inhibitor of Factor B, Has Superior Efficacy to Intravenous Terminal Complement Inhibition with Standard of Care Eculizumab or Ravulizumab and Favorable Safety in Patients with Paroxysmal Nocturnal Hemoglobinuria and Residual Anemia: Results from the Randomized, Active-Comparator-Controlled, Open-Label, Multicenter, Phase III Apply-PNH Study. Late-Breaking Abstract 2, ASH 64th Annual Meeting, 10–13 December 2022, New Orleans, LA, USA.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Novel therapy may replace standard-of-care prophylaxis for GVHD Next Article
Neutrodiet: non-restricted diet is the preferred option after SCT »
« Novel therapy may replace standard-of-care prophylaxis for GVHD Next Article
Neutrodiet: non-restricted diet is the preferred option after SCT »
Table of Contents: ASH 2022
Featured articles
Acute Lymphoblastic Leukaemia
Blinatumomab candidate for standard-of-care in newly diagnosed B-ALL
High-dose methotrexate or standard interim maintenance in young patients with ALL?
Acute Myeloid Leukaemia
Excellent results for triplet regimen in FLT3-mutated AML
MRD by qPCR prognostic of outcomes in venetoclax-treated NPM1-mutated AML
Promising results for triplet therapy with magrolimab in AML
Should we use intensive chemotherapy prior to allo-HCT in relapsed/refractory AML?
Chronic Leukaemia
Zanubrutinib wins battle of BTK inhibitors in relapsed or refractory CLL/SLL
Ibrutinib plus venetoclax displays long-term benefits in CLL
Multiple Myeloma
Talquetamab further investigated in heavily pre-treated MM after promising phase 2 data
Promising results of elranatamab for MM in phase 2 MagnetisMM-3 trial
Deep and durable responses for quadruple therapy in smouldering MM
Ultra-sensitive MRD assessment in MM with BloodFlow
CAR-Hematotox score proves useful in relapsed/refractory MM
Head-to-head: VMP versus Rd in transplant-ineligible MM
Lymphoma
Ibrutinib added to ASCT improves clinical outcomes in mantle cell lymphoma
High-dose chemotherapy plus ASCT superior to standard immuno-chemotherapy in primary CNS lymphoma
Odronextamab has considerable anti-tumour effects in relapsed/refractory diffuse large B-cell lymphoma and follicular lymphoma
Excellent results for AFM13-complexed NK cells in CD30-positive lymphoma
CAR-Hematotox score predicts toxicity, infections, and clinical outcomes in MCL
Myeloproliferative Neoplasms
Efgartigimod successful in immune thrombocytopenia
INCA033989: novel investigational agent for CALR-mutated MPN
Ruxolitinib mediates clonal evolution of RAS pathway mutations in MPN
Immune Thrombocytopenia
Long-term risk for haematologic disease in persistent, isolated mild thrombocytopenia
Various Topics
C1 inhibitor deficiency linked to thrombosis
Durable responses to gene therapy in haemophilia A
Long-term benefits from beti-cel in transfusion-dependent β-thalassaemia
Neutrodiet: non-restricted diet is the preferred option after SCT
Iptacopan offers solution for patients with PNH and residual anaemia after standard-of-care
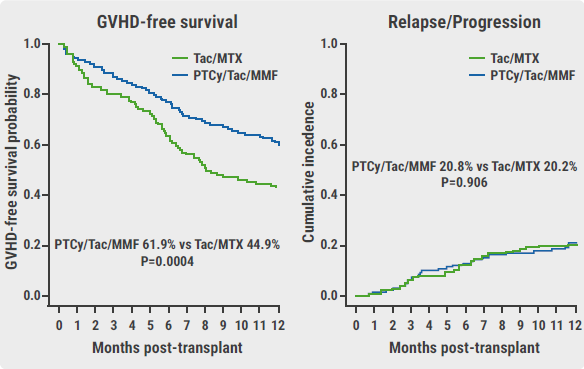
Novel therapy may replace standard-of-care prophylaxis for GVHD
LMWH does not result in higher live birth rates in women with inherited thrombophilia
Related Articles
February 20, 2023
Novel therapy may replace standard-of-care prophylaxis for GVHD
February 20, 2023
C1 inhibitor deficiency linked to thrombosis
February 20, 2023
Durable responses to gene therapy in haemophilia A
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

