https://doi.org/10.55788/2e502088
Although SC infliximab has been studied as an alternative to IV infliximab to maintain remission in patients with IBD, SC infliximab in high-risk patients or in those who had been treated with IV infliximab for a long period has not yet been evaluated. The current retrospective cohort study involved 306 participants in clinical remission, either high-risk patients or patients who had been on IV infliximab for a longer duration [1]. The efficacy, pharmacokinetics, and safety of SC infliximab were analysed compared with its IV counterpart. The study assessed objective biomarkers and clinical disease activity scores, ensuring a comprehensive evaluation of the drug’s performance over various periods.
The participants on SC infliximab demonstrated remarkable treatment persistence, with an 87% rate compared with 35% in the IV group (P<0.001). The SC infliximab group also exhibited a significant increase in drug levels (OR 31.77; P=0.001) and a decrease in treatment discontinuation rate due to anti-drug antibody formation (2% vs 20%, in the SC and IV groups, respectively) and side effects (3% vs 13%, respectively).
The findings advocate considering SC infliximab as a viable and effective alternative for patients in established clinical remission on IV infliximab. One of the researchers elaborated on the study’s findings: "Subcutaneous switch should be considered in patients in established clinical remission on IV infliximab as offering an effective and safe alternative in IBD. Subcutaneous switch should even be considered in those high-risk patient groups." The SC route has shown favourable pharmacokinetic properties, heralding a new era in the personalised-treatment approach in IBD.
- Mahmood T, et al. A retrospective cohort study to compare the efficacy, pharmacokinetics and safety of subcutaneous (SC) and intravenous (IV) infliximab in the treatment of inflammatory bowel disease. LB02, UEG Week 2023, 14–17 October, Copenhagen, Denmark.
Copyright ©2023 Medicom Medical Publishers
Posted on
Previous Article
« Safer removal of large polyps with cold snare technique Next Article
ARTEMIS-UC: New kid in town for UC »
« Safer removal of large polyps with cold snare technique Next Article
ARTEMIS-UC: New kid in town for UC »
Table of Contents: UEGW 2023
Featured articles
SEQUENCE: Risankizumab doubles endoscopic remission rates compared with ustekinumab in CD
What’s New in Artificial Intelligence
Digital intervention relieves symptoms and improves QoL in IBS
GastroGPT: Successful proof-of-concept study of gastroenterology-specific large language model
Other Therapeutics and Outcomes
Primary results from MAESTRO-NASH trial: resmetirom efficacious for NASH
Apraglutide: Advancing the treatment of short bowel syndrome
Endobiliary radiofrequency ablation in pCCA: a pilot study
Raising awareness for microscopic colitis: disease course and predictors
Outcomes of IBD Trials
DIVERSITY1: Filgotinib results in Crohn’s disease leave investigators puzzled
SEQUENCE: Risankizumab doubles endoscopic remission rates compared with ustekinumab in CD
Guselkumab provides benefits in UC regardless of advanced therapy history
INSPIRE: Risankizumab meets all efficacy endpoints in UC
Risankizumab resolves extraintestinal manifestations in CD
Obefazimod takes the spotlight as promising UC treatment
Rapid response to upadacitinib boosts outcomes in severe Crohn’s disease
LUCENT trials: Mirikizumab works in UC, regardless of targeted therapy history
ARTEMIS-UC: New kid in town for UC
Breakthroughs in Colorectal Lesions
Safer removal of large polyps with cold snare technique
Higher recurrence rates with cold snare EMR than with conventional EMR
How to deal with at-risk patients above the CRC screening age limit?
European CRC screening needs to be revised
Advances in Upper Endoscopy and Colonoscopy
Epinephrine boosts efficiency in gastric ESD
Artificial intelligence-aided colonoscopy did not improve outcomes in Lynch syndrome
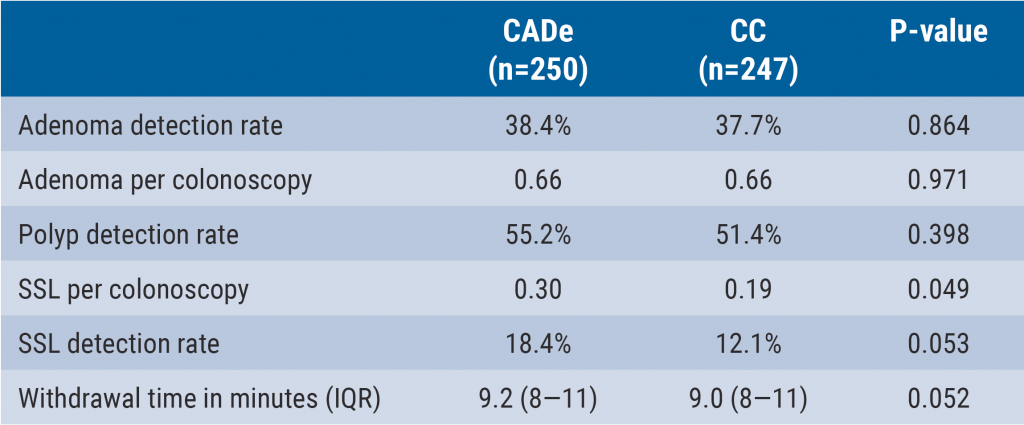
Can computer technology improve our everyday colonoscopy results?
Is AI-assisted colonoscopy ready for clinical practice?
Should we use E-SEMS or EVT for traumatic oesophageal perforations?
Related Articles
December 7, 2023
Is AI-assisted colonoscopy ready for clinical practice?
December 7, 2023
Can computer technology improve our everyday colonoscopy results?
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

