The authors suggest screening for and treating these disorders to improve outcomes.
"I would stress the onus would be on the GI physician to screen, but then to refer on to a psychiatrist or psychologist for consideration of treatment," Dr. Alexander Ford of the University of Leeds, UK told Reuters Health by email.
But "in a busy, fee-based, procedure-driven specialty like gastroenterology in the U.S., where it is not incentivized to address these issues as part of the consultation, it may be unlikely to happen," he acknowledged.
As reported in The Lancet Gastroenterology and Hepatology, Dr. Ford and colleagues searched the literature through September 2020 for observational studies with at least 100 IBD patients that reported prevalence of anxiety or depression symptoms.
Seventy-seven studies (of 5,544) involving more than 30,000 patients were included. Overall, the pooled prevalence of anxiety symptoms was 32.1% (58 studies) and of depression symptoms, 25.2% (75 studies).
In studies that reported the prevalence in Crohn's disease and ulcerative colitis within the same population, those with Crohn's disease had higher odds of anxiety and depression symptoms (OR, 1.2 for both).
Overall, women with IBD were more likely than men to have symptoms of anxiety (pooled prevalence, 33.8% vs. 22.8%; OR 1.7) and depression (pooled prevalence, 21.2% vs. 16.2%; OR 1.3).
Further, the prevalence of symptoms was higher in patients with active versus inactive IBD: 57.6% versus 38.1% (OR, 2.5) for anxiety and 38.9% versus 24.2% (OR, 3.1) for depression.
Dr. Laurie Keefer, Director for Psychobehavioral Research at the Icahn School of Medicine at Mount Sinai in New York City, author of a related editorial, commented by email to Reuters Health, "We have a significant problem in IBD management - even though medical therapies are improving, patients continue to struggle with the emotional sequelae of having a chronic, stigmatizing illness."
At every visit, she said, gastroenterologists should be asking patients directly, "How are you managing emotionally?" Open-ended questions like this "will surface many other worries and concerns that patients with IBD report," she added, "including lack of disease acceptance or knowledge; low confidence in their ability to manage everything; lack of social support; or concerns around intimacy, body image, fatigue, sleep difficulties, and fear of symptoms. Patients may even report medical trauma when asked this question."
"Patients do not expect that their GI doctors will solve these issues for them, and it can be very therapeutic for them to even know that their doctor cares or empathizes with their situation," she noted. "Usually, these discussions only take an extra minute or two but are really high-value to both the patient and provider. If you are running short on time, you can also always validate the concern and set up a separate appointment to discuss in more detail."
SOURCE: https://bit.ly/31fktqG and https://bit.ly/2NOUpiZ Lancet Gastroenterology and Hepatology, online March 12, 2021.
By Marilynn Larkin
Posted on
Previous Article
« Substantial discordance between troponin assays for ACS risk stratification Next Article
Pfizer’s atopic dermatitis drug bests dupilumab, but only at higher dose »
« Substantial discordance between troponin assays for ACS risk stratification Next Article
Pfizer’s atopic dermatitis drug bests dupilumab, but only at higher dose »
Related Articles
April 18, 2024
Novel agent VTX002 holds promise in ulcerative colitis
April 14, 2020
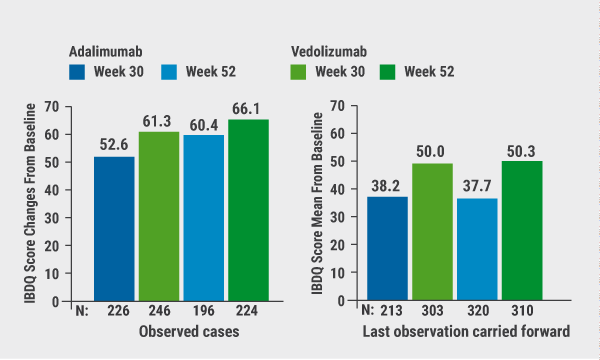
Effects of vedolizumab versus adalimumab on QoL
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

