"Although these results are disappointing, it might be premature to dismiss etrolizumab therapy in ulcerative colitis without further study, caution Dr. Manasi Agrawal of Mount Sinai Health Systems, in New York City, and Dr. Bram Verstockt of University Hospitals Leuven, in Belgium, in a linked comment.
Etrolizumab is being developed by F Hoffman-La Roche, which funded the studies, all published in The Lancet Gastroenterology & Hepatology.
Etrolizumab is a dual-action anti-beta-7 monoclonal antibody that selectively targets both alpha-4-beta-7 and alpha-E-beta-7 integrins to control both trafficking of immune cells into the gut and their inflammatory effects on the gut lining.
HIBISCUS I and HIBISCUS II were two identical, randomized, placebo-controlled trials comparing etrolizumab with placebo and adalimumab in patients with moderately to severely active UC who had never been treated with a tumor necrosis factor (TNF) inhibitor.
The proportion of patients achieving remission at week 10 was significantly higher with etrolizumab than with placebo in HIBISCUS I, but not in HIBISCUS II. In a pooled analysis, etrolizumab was not superior to adalimumab, the investigators report.
HICKORY was a placebo-controlled induction and maintenance study of patients with previous exposure to TNF inhibitors. In this trial, a significantly higher proportion of patients treated with etrolizumab achieved remission at 14 weeks compared with placebo; however, there was no significant difference between groups in remission at 66 weeks among patients who responded at 14 weeks.
GARDENIA was a randomized study comparing etrolizumab with infliximab in patients with moderately to severely active UC with no prior TNF-inhibitor exposure.
In this study, etrolizumab was not superior to infliximab on the primary endpoint (the proportion of patients who had both clinical response at week 10 and clinical remission at week 54). From a clinical viewpoint, etrolizumab performed similarly to infliximab, the investigators report.
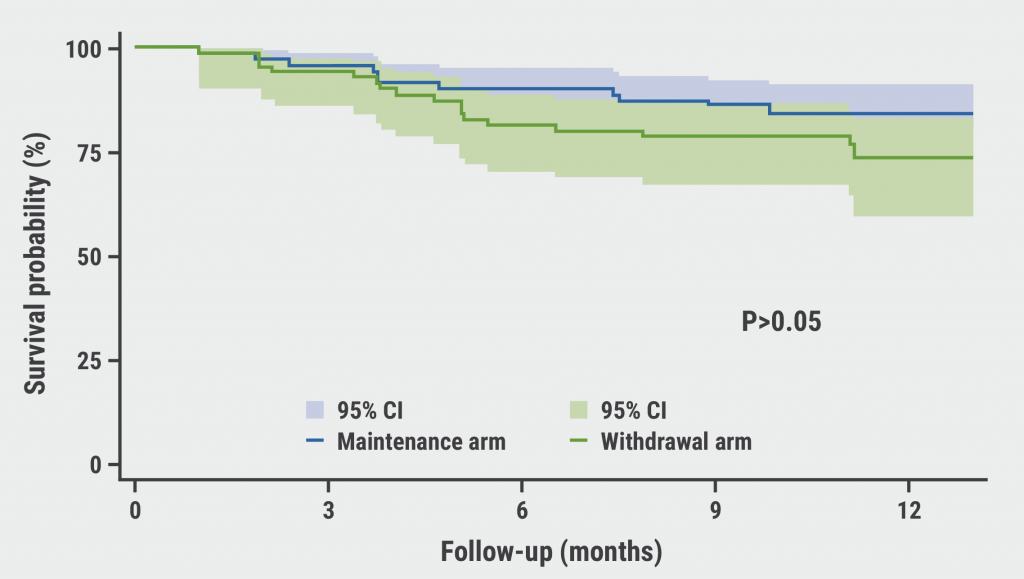
LAUREL was a randomized, placebo-controlled, maintenance study comparing etrolizumab with placebo in patients with moderately to severely active UC with no prior TNF-inhibitor exposure.
In this study, there were no significant differences between maintenance etrolizumab and placebo in the primary endpoint of remission at 62 weeks among who had a clinical response at 10 weeks.
In all five studies, etrolizumab was well tolerated with no new safety signals.
The comment authors offer several caveats to these trials for consideration.
"Although remission rates with etrolizumab were lower than originally anticipated based on phase 2 data, the induction data are consistent with a clinical remission rate in TNF inhibitor-naive (HIBISCUS I and II) and TNF inhibitor-exposed patients (HICKORY) of approximately 20%," they point out.
"The finding that etrolizumab, while not superior to placebo in HIBISCUS, LAUREL, and HICKORY was associated with similar proportions of patients reaching remission as with TNF inhibitors in HIBISCUS (adalimumab; exploratory endpoint) and GARDENIA (infliximab; primary endpoint) is also encouraging," they say.
Drs. Agrawal and Verstockt add that "some reasons postulated for the negative results include an ambitious effect size assumption and high placebo response rates. A low dose of etrolizumab (105 mg subcutaneous once every 4 weeks) was studied across all trials."
The studies also lacked information on baseline integrin alpha-E expression as a predictive biomarker.
"Moving forward, recruiting a molecularly enriched subgroup of patients could result in a significantly larger difference between treatment groups and allow for a smaller sample size (and reduced associated resources) without compromising on power," Drs. Agrawal and Verstockt suggest.
"Although etrolizumab is currently far from approval as a treatment option in ulcerative colitis, the current data are provocative and highlight questions to be addressed in post-hoc analyses, and data from Crohn's disease trials (BERGAMOT and JUNIPER) are awaited," they add.
SOURCE: https://bit.ly/30PKD6o, https://bit.ly/3CL04tK, https://bit.ly/30O6ICm, https://bit.ly/3cXnORf, https://bit.ly/3l2Jlwh The Lancet Gastroenterology & Hepatology, online November 16, 2021.
By Reuters Staff
Posted on
Previous Article
« Smartphone app shows promise in easing symptoms of severe mental illness Next Article
Maintenance olaparib benefits sustained beyond 2 years treatment »
« Smartphone app shows promise in easing symptoms of severe mental illness Next Article
Maintenance olaparib benefits sustained beyond 2 years treatment »
Related Articles

April 14, 2020
Impact of strategies on intestinal resection rate
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

