"The take-home message at the moment is that melanoma surgeons should talk to their breast cancer surgeon colleagues to prepare themselves for this likely upcoming new approach of surgery in stage III melanoma," Dr. Christian Blank of The Netherlands Cancer Institute in Amsterdam told Reuters Health by email.
"The PRADO trial (https://bit.ly/3gLFZLo) results that we hope to present at ASCO 2022 this June prospectively tested the ILN procedure, using the results to de-escalate in good responders and to escalate therapy in non-responders," he said.
Dr. Blank and colleagues note in JAMA Surgery that neoadjuvant checkpoint inhibition in patients with high-risk stage III melanoma shows high pathologic response rates associated with a durable relapse-free survival. A previous small pilot study with 12 patients showed that the response in the ILN may be representative of the pathologic response in the entire TLND specimen.
The current analysis included 82 patients (median age, 58.5; 59%, male) enrolled in two separate trials who were treated with neoadjuvant ipilimumab and nivolumab followed by TLND.
The pathologic response in the ILN was concordant with the entire TLND specimen response in 81 patients (99%), and it was concordant in 79 (96%) when comparing the ILN response with the response in every individual lymph node.
In one patient, the ILN response (20% viable tumor, partial pathologic response) underestimated the entire TLND specimen response (5% viable; near-complete pathologic response). Two other patients each had one small non-index node that contained 80% viable tumor (pathologic nonresponse), whereas all other lymph nodes (including the ILN) showed a partial pathologic response; for these patients, the risk of regional relapse potentially might have been increased if TLND had been omitted.
The ILN showed a complete pathological response in 34 patients (41%); a near-complete response in 15 (18%); and a partial response in 11 (13%). The entire TLND specimen showed a complete response in 34 patients (41%); a near-complete response in 16 (20%); and a partial response in 10 (12%).
The authors conclude, "The results of this study suggest that the pathologic response of the ILN may be considered a reliable indicator of the entire TLND specimen response and may support the ILN response-directed omission of TLND in a prospective trial."
Dr. Sandra Wong of the Geisel School of Medicine at Dartmouth in Lebanon, New Hampshire, coauthor of a related editorial, commented in an email to Reuters Health, "This is a timely report because use of neoadjuvant treatment continues to expand and with effective treatments, questions about need for surgical resection - or at least the extent of resection - will continue to arise."
"One important lesson from our experience with sentinel lymph node (SLN) biopsy is that there is no benefit to removing uninvolved lymph nodes, so assurance that there are no occult cells in the ILN is critical," she said. "One consideration with the data presented is that immunohistochemical analysis of the ILN did not appear to be used."
"Further, we know that minimizing false negative SLN results is important," she noted. "The authors acknowledge that the ILN may not be the same node that was biopsied before neoadjuvant treatment and this could be a source of false negative results - i.e., that the ILN is not truly representative of the status of the nodal basin."
"Despite this limitation, these results inform practice while we await results from the ongoing PRADO study," she said.
"What we have more recently learned with our SLN biopsy experience is that the sentinel node may be the only involved node (or nodes)," she added. "Again, there is no benefit to removing uninvolved nodes, so it is noteworthy that removing the ILN may be therapeutic as well as diagnostic. This could be a future direction as we continue to advance neoadjuvant treatment and consider ways to be more precise about surgical procedures."
SOURCE: https://bit.ly/3rTvigm and https://bit.ly/3Bl7p4l JAMA Surgery, online February 9, 2022.
By Marilynn Larkin
Posted on
Previous Article
« Cold-snare polypectomy safe if DOACs withheld on day of procedure Next Article
Multiple sleep problems may boost heart disease risk by more than 140% »
« Cold-snare polypectomy safe if DOACs withheld on day of procedure Next Article
Multiple sleep problems may boost heart disease risk by more than 140% »
Related Articles
December 20, 2018
CNNs and targeted combination therapy
August 12, 2021
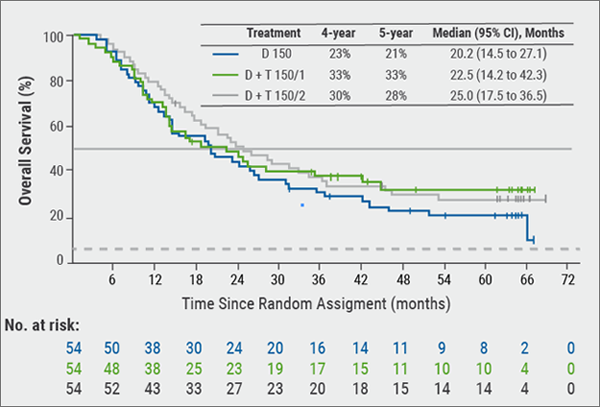
Long-term results from ground-breaking melanoma trials

November 5, 2022
Markedly lower skin cancer risk in vitiligo patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

