https://doi.org/10.55788/d60ea6c6
The reported prevalence of genital psoriasis or psoriasis in other areas of sexual interest in individuals already diagnosed with psoriasis varies widely in the literature (17–64%) [1‒4]. Dr Toni Klein (University Medical Center Hamburg-Eppendorf, Germany) wished to further explore the prevalence of genital psoriasis and its impact on patients’ sexual life [5].
A cross-sectional survey was conducted by sending questionnaires to a random sample of patients registered in the PsOBest registry (NCT01848028) in Germany. Included in the questionnaires were the Genital Psoriasis Symptom Scale (GPSS), which evaluates the severity of 8 genital psoriasis symptoms and the Genital Psoriasis Sexual Impact Scale (GPSIS), which assesses whether patients avoid sexual activity because of genital psoriasis and level of worsening of genital psoriasis symptoms following sexual activity. Moreover, the researchers included questions exploring both generic and psoriasis-specific reasons for sexual impairment (RSI).
From the 2,010 questionnaires that were sent out, the team received 811 responses (40.3%) and analysed 795 (39.6%). Of these, 41.9% were filled in by women, 51.6% by men, and 6.5% did not report their gender. The mean age at onset of psoriasis was 26.6 years and the mean age for the onset of genital psoriasis was 35.0 years, and for psoriasis in other areas of sexual interest 34.1 years.
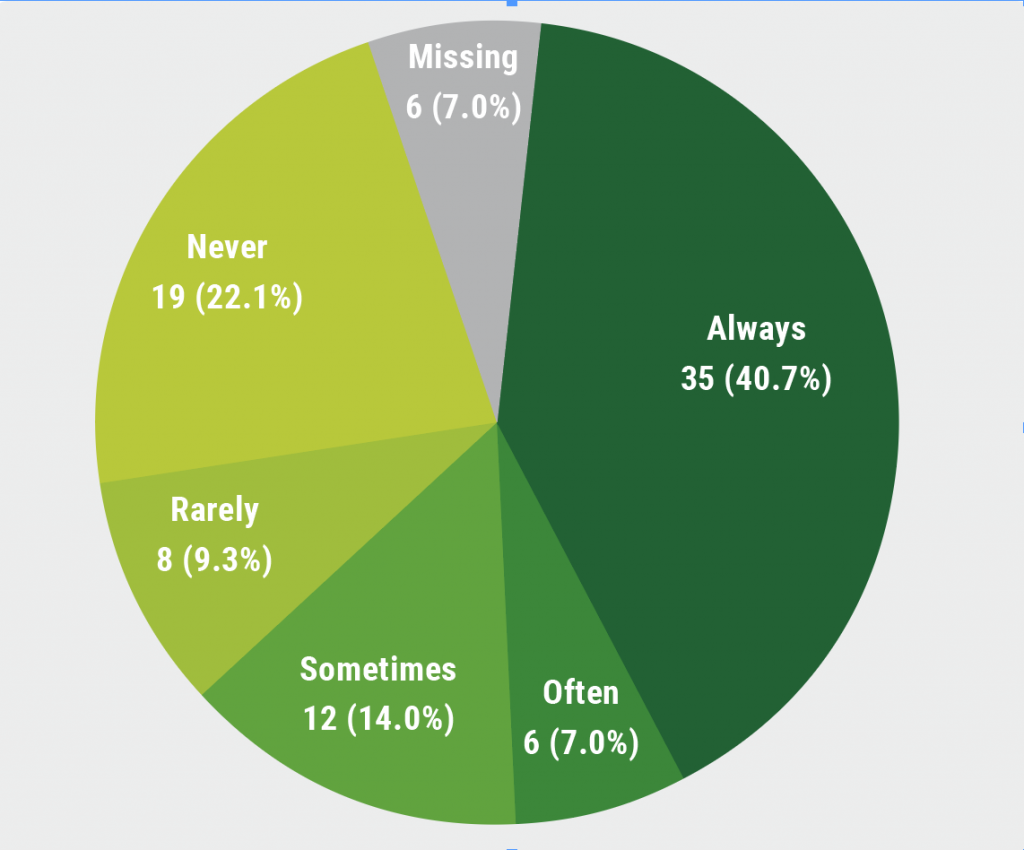
During the previous 24 months, 1/5 participants experienced genital psoriasis, whilst nearly half experienced psoriasis in any other areas of sexual interest. Genital psoriasis and psoriasis at any ASI had a remarkable impact on sexual function: A majority of participants with genital psoriasis suffered from sexual impairment in the last 30 days and this led to 12.8% of participants avoiding sex altogether, and 40.7% of participants avoiding sex during the last week (see Figure). Despite its high impact, only a quarter of these participants discussed having sexual impairments with their dermatologists.
Figure: Proportion of genital psoriasis patients avoiding sexual activities within the past week [5]
Dr Klein and her team concluded that dermatologists should be aware of the high prevalence of genital psoriasis. Therefore, genital areas shouldn’t be neglected when examining patients as psoriasis in this location impairs quality-of-life and often leads to sexual dysfunction.
- Da Silva N, et al. Eur J Dermatol 2020;30:267‒78.
- Da Silva N, et al. J Eur Acad Dermatol Venereol 2020;34:1010‒1018.
- Da Silva N, et al. PLos Online 2020;15:e0235091.
- Augustin M, et al. Br J Dermatol 2019;181:358‒65.
- Klein TM, et al. Epidemiological Survey on the Prevalence of Genital Psoriasis and Its Impact on Patients’ Sexual Life in Routine Care. P1564, EADV Congress 2022, Milan, Italy, 7–10 September.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Decreased overall survival in melanoma patients with low vitamin D Next Article
High rate of non- or partial responders jeopardises therapeutic success in HS »
« Decreased overall survival in melanoma patients with low vitamin D Next Article
High rate of non- or partial responders jeopardises therapeutic success in HS »
Table of Contents: EADV 2022
Featured articles
Letter from the Editor
Psoriasis and Psoriatic Arthritis: What You Need to Know
Novel oral psoriasis drug maintains efficacy over 2 years
A3 adenosine receptor agonist showed modest efficacy but excellent tolerability
Selective IL-23 inhibitor achieves long-term disease control in many patients with active PsA
AI machine learning algorithm useful in early detection of PsA
Novel Developments in Sun Protection
Myths regarding “health benefit” of suntan prevail in majority of population
Fern extract reverses severe actinic keratosis lesions
Vitiligo in 2022
Enhancing re-pigmentation rates with topical ruxolitinib in all body areas
Markedly lower skin cancer risk in vitiligo patients
Pruritus Treatment: Novel Agents Entering the Arena
Dupilumab leads to clinically relevant improvements in signs and symptoms of prurigo nodularis
Nalbuphine: aspiring to become another treatment for prurigo nodularis?
Notalgia paresthetica: may κ-opioid receptor agonists be a long-awaited effective therapy?
Pharmacotherapy in Hidradenitis Suppurativa: New Opportunities
High potential for secukinumab as next biologic treatment for HS
Hidradenitis suppurativa: TYK2/JAK1 inhibitor shows promise
Best of the Posters
High rate of non- or partial responders jeopardises therapeutic success in HS
Genital psoriasis: high prevalence, often underdiagnosed
Decreased overall survival in melanoma patients with low vitamin D
News in Atopic and Seborrheic Dermatitis
Baricitinib possible therapeutic option for children with AD
Amlitelimab therapy leads to sustained decrease of IL-22 in AD patients
IL-13 inhibition with lebrikizumab shows high maintenance rates in AD
Does 8 weeks of emollients use prevent AD in high-risk infants?
Roflumilast foam led to high response rates in seborrheic dermatitis
What Is Hot in Hair Disorders?
Long-term improvement in alopecia areata with ritlecitinib therapy
Topical gel plus finasteride beneficial for patients with androgenetic alopecia
Deuruxolitinib achieves hair regrowth, even in patients with severe alopecia areata
Related Articles
November 5, 2022
Long-term improvement in alopecia areata with ritlecitinib therapy
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

