https://doi.org/10.55788/8d5ad21b
With more and more biologics entering the therapeutic arena, it is important to know the consequences of switching between biologics. As Prof. Richard Warren (University of Manchester, UK) pointed out, data from the phase 3 aIMM study (NCT04102007) “gives us a very clear definition of suboptimal response and the very clear benefit of switching to risankizumab, offering further scientific proof when considering treatment options for patients”.
In the open, single-arm study, all included patients (n=252) had to be on an IL-17 blocker (i.e. secukinumab or ixekizumab) for at least 6 months and show a suboptimal response (defined as static Physicians’ Global Assessment [sPGA] 2/3 and body surface area affected 3% to <10%) on treatment. They were then treated with 150 mg risankizumab at weeks 0, 4, and every 12 weeks through week 40 without a washout period. “That reflects reasonably what we do in clinical practice,” Prof. Warren commented on the study design.
The primary study endpoint was the percentage of participants achieving a PGA 0/1 (i.e. clear or almost clear skin) at week 16 after switching. In addition, the percentage of participants achieving PGA 0, a Dermatology Life Quality Index of 0 (i.e quality of life no longer impaired by the disease), and Psoriasis Symptom Scale (PSS) scores were assessed at week 16 and 52 as secondary endpoints. “The mean disease duration was 20.8 years; this is a tough-to-treat population,” Prof. Warren said.
At week 16, 52% of the participants treated with risankizumab achieved the primary endpoint (sPGA 0/1). Moreover, participants demonstrated a numerical improvement in all endpoints between week 16 and week 52. “Between weeks 16 and 52, there is an accrual of each outcome,” Prof. Warren said. An sPGA of 0/1 was achieved by 63% of the participants and 46% achieved an Dermatology Life Quality Index (DLQI) scores of 0/1 (i.e. no effect on patient’s life). A PSS of 0 was achieved by 27.4% of participants at this time; a “hard-to-meet endpoint,” as Prof. Warren put it. No new safety signals were observed in this analysis.
- Warren R. Efficacy and safety after 52 weeks in psoriasis patients switching to risankizumab after suboptimal response to secukinumab or ixekizumab. S025, AAD 2023 Annual Meeting, 17–21 March, New Orleans, USA.
Posted on
Previous Article
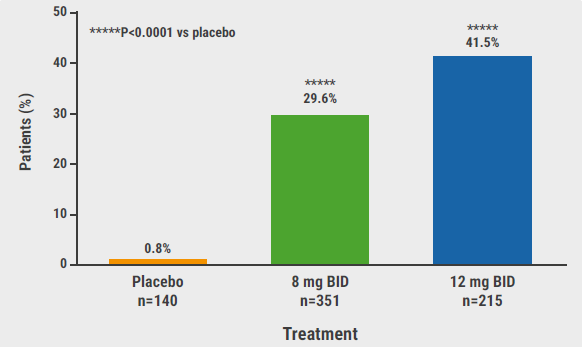
« Novel, selective TYK2 inhibitor shows promise for psoriasis Next Article
Bimekizumab could be the new up-and-comer for HS treatment »
« Novel, selective TYK2 inhibitor shows promise for psoriasis Next Article
Bimekizumab could be the new up-and-comer for HS treatment »
Table of Contents: AAD 2023
Featured articles
New Developments in Dermatology
Delgocitinib shows promise as topical therapy for chronic hand eczema
Vitiligo patients maintain re-pigmentation after ruxolitinib cream withdrawal
Nemolizumab decreases lesions and itch in prurigo nodularis
Lichen planus: a future indication for baricitinib?
Atopic Dermatitis: State of the Art
As-needed ruxolitinib shows successful long-term symptom control in AD
Dupilumab: a viable option for atopic hand and foot eczema
Topical roflumilast beneficial in atopic dermatitis
IL-22 receptor blocker reduces itch and skin lesions in AD
Psoriasis: New Developments
Switching to risankizumab successful in IL-17 inhibitor non-responders
Novel, selective TYK2 inhibitor shows promise for psoriasis
Hidradenitis Suppurativa: What You Need to Know
Izokibep shows remarkably high grades of clinical response in HS
Bimekizumab could be the new up-and-comer for HS treatment
Pearls of the Posters
Biologics in psoriasis: can they prevent joint involvement?
JAK inhibitor deuruxolitinib shows encouraging hair re-growth in alopecia areata
Biomarkers predicting response of different CSU treatments in children
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy