Therefore, applying proBNP cut points regardless of sex and race could lead to an underestimation of risk in Black men and an overestimate in white women, researchers say.
"NT-proBNP has been known to be lower in men compared to women, and lower in those identifying as Black race compared to White race," Dr. Amil Shah of Brigham and Women's Hospital in Boston told Reuters Health by email. "However, the risk of HF is generally higher in men and higher in Black individuals. Despite these differences, guideline-recommended thresholds for defining heart failure risk and heart failure vary by age but not sex or race."
"The main finding from our study was that, at any given NT-proBNP concentration, the absolute risk of developing HF varied substantially between groups defined by race and sex."
"NT-proBNP concentrations should be considered in the context of sex and race to allow for more uniform risk prediction," he said. "While we identified specific thresholds in our study population for each group defined by race and sex, future studies are needed to determine the generalizability of these specific thresholds."
As reported in JAMA Cardiology, Dr. Shah and colleagues analyzed data from the longitudinal Atherosclerosis Risk in Communities (ARIC) study to assess the association of NT-proBNP concentrations with relative and absolute risks of HF by sex and race at study visit 2 (1990-1992) and study visit 5 (2011-2013).
Participants were free of HF at visit 2 (midlife; 12,750) and at visit 5 (late life; 5,191).
The main outcome was incident HF or death.
Among those who were HF-free at visit 5, the mean age was 76; 41% were men; 20% were Black; and the median NT-proBNP concentration was 124 pg/mL.
In both midlife and late life, NT-proBNP concentrations were lowest in Black men (median, 30 at visit 2, and 74 pg/mL at visit 5) and highest in white women (median, 70 at visit 2 and 154 at visit 5).
Sex and race differences in NT-proBNP concentrations persisted after accounting for age, income, education, area deprivation index, cardiovascular diseases, left ventricular structure (LV), LV function, LV wall stress, weight and fat mass, and estimated glomerular filtration rate.
Substantial differences in the absolute risk of incident HF or death were seen across the sex- and race-based categories at any NT-proBNP concentration; for example, a 7-fold and 3-fold difference at visit 2 and 5, respectively, at guideline-recommended thresholds, with higher risk consistently observed among Black men and lower risk in white women.
The results were replicated in participants from the Cardiovascular Health Study.
JAMA Cardiology Deputy Editor Dr. Clyde Yancy and Dr. Sadiya Khan, both of Northwestern University Feinberg School of Medicine in Chicago, coauthored an accompanying editorial. They commented in a joint email to Reuters Health, "Investigators from the ARIC study carefully assessed NT-proBNP concentrations and the risk of developing HF as a function of sex and race."
"Not unsurprisingly, NT-proBNP levels did vary, but Black men especially were at a 7-fold higher risk of developing heart failure and at a lower NT-proBNP level," they said. "Race does not infer biology and is not a proxy for genetics. And any simple univariate analysis based on race should be considered inadequate, with the findings more likely to misdirect than inform."
"However, by adjusting for the social determinants of health and genetic ancestry, the residual risk attributable to self-identified race alone remains, but is much less," they noted. "The takeaway? No single threshold of NT-proBNP consistently associates with the risk of HF and both sex and race matter."
"Yet," they added, "the complexity of race requires more careful analysis to understand the drivers of risk. Credit the investigators for delving into this much more thorough analysis of race as a variable in health and disease."
SOURCE: https://bit.ly/3872euq and https://bit.ly/39nMUtJ JAMA Cardiology, online April 27, 2022.
Posted on
Previous Article
« FDA approves Bristol Myers’ oral heart disease drug Next Article
Proton-beam therapy increasingly popular in the U.S. »
« FDA approves Bristol Myers’ oral heart disease drug Next Article
Proton-beam therapy increasingly popular in the U.S. »
Related Articles
July 28, 2022
HELIOS-A: Vutrisiran meets exploratory endpoints
October 27, 2022
Dapagliflozin DELIVERs for HFmrEF/HFpEF
July 28, 2022
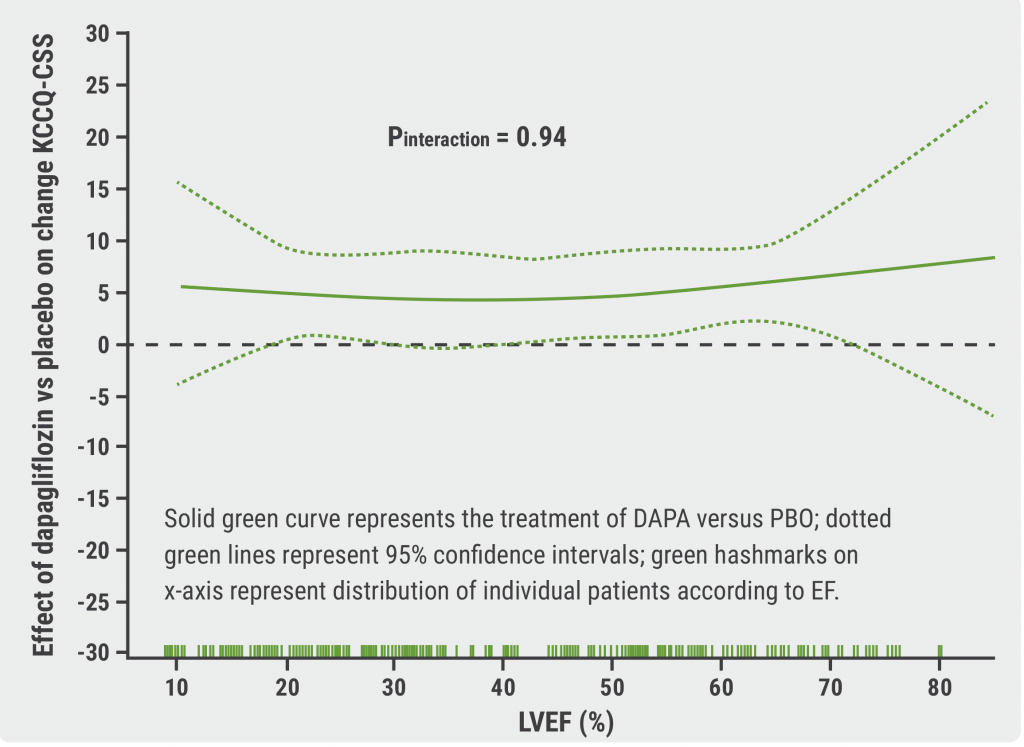
Dapagliflozin performs consistently across LVEF in HF
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

