https://doi.org/10.55788/6e8de9aa
“Ghrelin is a peptide hormone, that stimulates the release of growth hormone via the growth hormone secretagogue receptor and triggers appetite centrally,” outlined Prof. Lars Lund (Karolinska Institutet, Sweden) [1]. Since ghrelin receptors are widely distributed in people, including the vasculature and myocardium, and ghrelin is elevated in patients with HFrEF, Prof. Lund and colleagues aimed to test whether intravenous acyl ghrelin can increase the cardiac output of patients with HFrEF. For this purpose, the phase 2 MetAnEnd-HF trial (NCT05277415) randomised 30 patients with New York Heart Association (NYHA) class III or IV HFrEF 1:1 to receive a placebo infusion or ghrelin intravenously for 120 minutes. The cardiac output was measured continuously via inert gas rebreathing.
After 120 minutes of infusion, the mean cardiac output was significantly increased in participants who received ghrelin (4.08 L/min to 5.23 L/min; Pinteraction with time<0.001), representing a 28% increase in the cardiac output in participants on ghrelin, compared with participants who received placebo, in whom the cardiac output decreased slightly over time (4.26 L/min to 4.11 L/min; see Figure). Secondary efficacy outcomes, including left ventricular ejection fraction (LVEF), tricuspid annular plane systolic excursion (TAPSE), strain rate, and stroke volume, all favoured the experimental arm over the placebo arm numerically, but only the increase in stroke volume was significant over time (54.3 mL to 62.2 mL; Pinteraction with time=0.021).
Figure: Primary outcome measure—change in cardiac output [1]

The safety analysis showed that ghrelin was not associated with hypotension, tachycardia, arrhythmia, or ischaemia. However, in the ghrelin group, almost half of the participants experienced flushing. Also, the NT-proBNP levels of participants on ghrelin were slightly elevated after 2–5 days (2,080 ng/L to 2,450 ng/L; P=0.01). Furthermore, analysis of ex-vivo beating cardiomyocytes displayed that ghrelin increased the contractility in a load-independent fashion and that the effect of ghrelin was calcium-sensitising rather than calcium-inducing.
“These results show that ghrelin, with its mechanism of action, has potential as a safe inotrope/myotrope therapy for the treatment of patients with HFrEF,” concluded Prof. Lund.
- Lund LH, et al. Ghrelin-HF: intravenous ghrelin in heart failure with reduced ejection fraction. LBT Pharmacotherapy, Heart Failure 2022, 21–24 May, Madrid, Spain.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« Combination of filgrastim and dutogliptin appears safe in STEMI Next Article
SERENADE: Macitentan fails in HFpEF plus PAH »
« Combination of filgrastim and dutogliptin appears safe in STEMI Next Article
SERENADE: Macitentan fails in HFpEF plus PAH »
Table of Contents: HFA 2022
Featured articles
Phase 3 and 4 Trials
GALACTIC-HF: Omecamtiv mecarbil as option for HFrEF patients with low SBP
HELIOS-A: Vutrisiran meets exploratory endpoints
Patiromer helps HFrEF patients to optimise RAAS inhibitors without hyperkalaemia
FIDELITY: Cardiorenal benefits of finerenone, regardless of LVH status
DAPA-VO2: Rapid effect of dapagliflozin on peak VO2 in stable HFrEF
Phase 1/2 Trials
Significant improvement in BP from istaroxime, a novel non-adrenergic agent
SERENADE: Macitentan fails in HFpEF plus PAH
Combination of filgrastim and dutogliptin appears safe in STEMI
Therapeutic Devices
Cardiac contractility modulation therapy promising for patients with HFpEF
REBALANCE-HF: Encouraging observations for splanchnic nerve ablation in HFpEF
Updates on SGLT2 Inhibitors
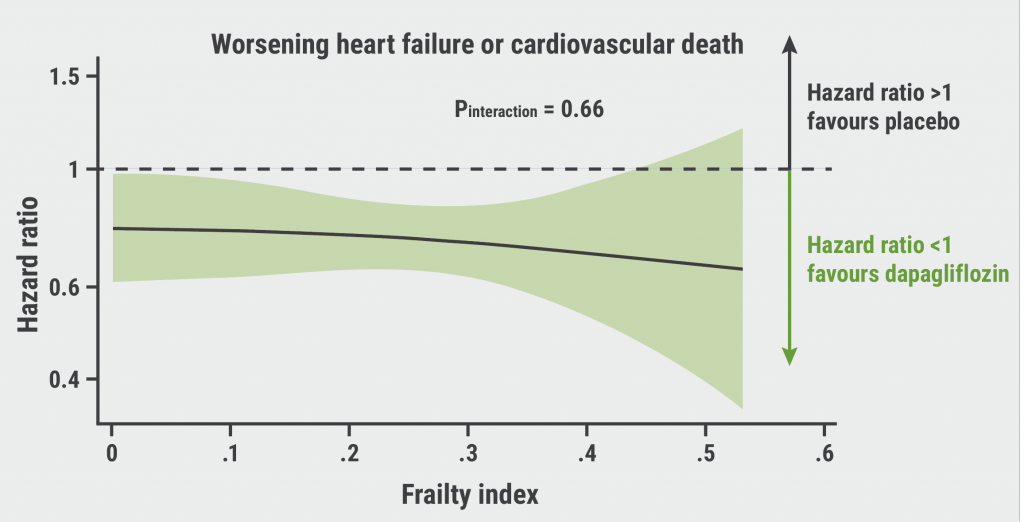
DAPA-HF: Dapagliflozin is safe and efficacious in frail patients
EMPEROR-Preserved: Empagliflozin stable across age groups
EMPULSE: Empagliflozin delivers rapid and clinically meaningful decongestion
Dapagliflozin performs consistently across LVEF in HF
Miscellaneous Topics
Cardiac wasting relevant for clinical outcomes in cancer
Urocortin-2 a potential treatment target for HFpEF
Should ATTR-CM be added to the differential diagnosis of patients with HF?
Delayed initiation of novel GDMTs associated with adverse outcomes in HF patients
Related Articles
October 27, 2022
No effect of neprilysin inhibition on cognition
December 3, 2020
SGLT2 inhibitor reduces filling pressure in HFrEF patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

