“As the population is ageing, hypertension management among older patients has been increasingly discussed,” said Prof. Jun Cai (FuWai Hospital, China) pointing out that previous trials led to distinct conclusions. “This study is important because it addresses a very simple question: When treating BP in older people, how low should we go?” expressed the trial discussant Prof. Bryan Williams (University College London, UK) [3].
STEP (NCT03015311) investigated intensive BP treatment from 110 mmHg to <130 mmHg as SBP target versus standard therapy with SBP between 130 mmHg and <150 mmHg. The study enrolled 8,511 patients between 60–80 years of age who had no history of a prior stroke. BP medications consisted of olmesartan, amlodipine, and hydrochlorothiazide. The measuring of BP was either performed by trained personnel in an office setting or at home with a smartphone app as a monitoring device. Furthermore, various examinations were executed at baseline and throughout the control visits including ECG, echocardiography, and cognitive function testing.
The primary outcome was a composite of multiple adverse CV events (i.e. stroke, acute coronary syndrome, revascularisation, decompensation of heart failure, atrial fibrillation, CV mortality). Baseline findings of the study population included a mean age of 66.2 years, just over half of the participants were women, and about 19% had diabetes.
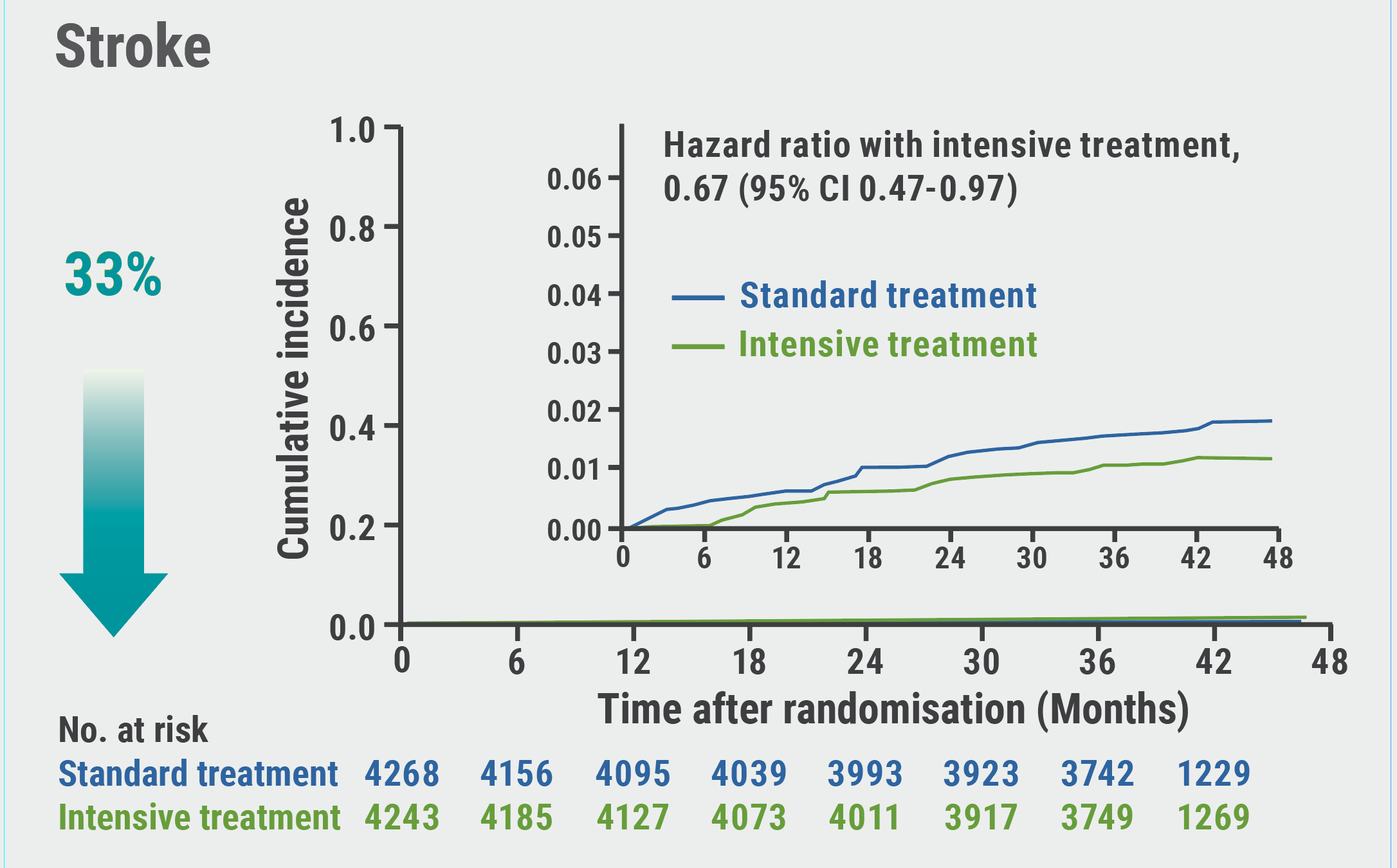
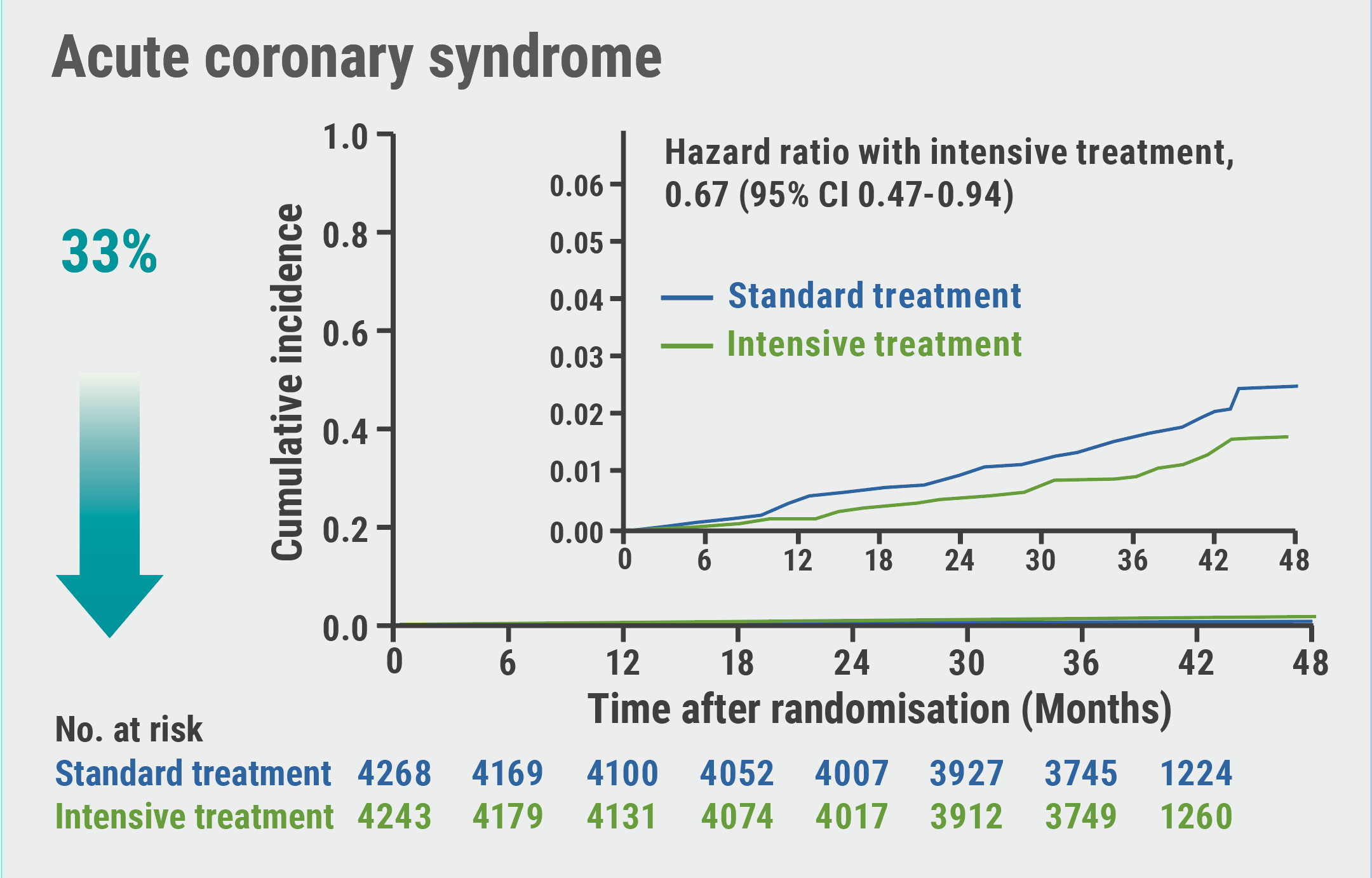
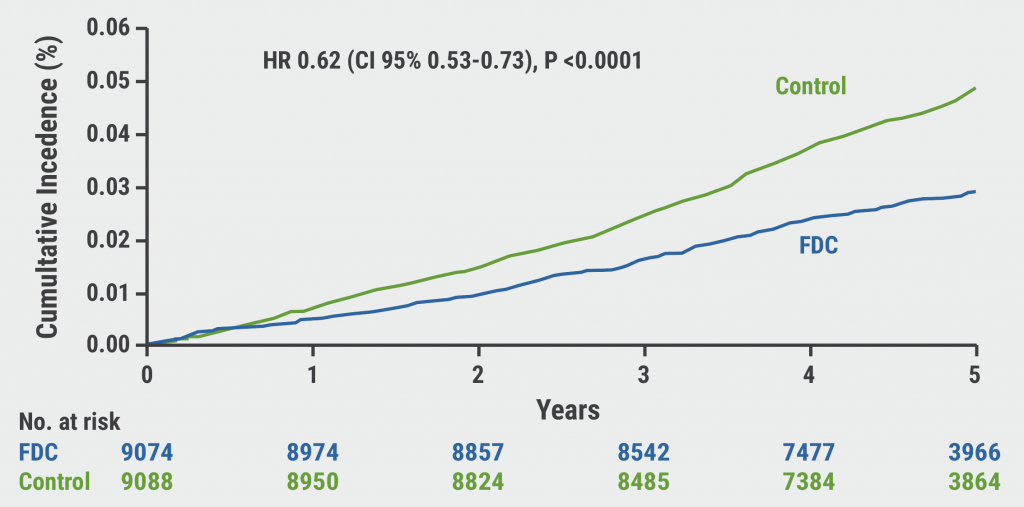
“After randomisation, the 2 treatment strategies resulted in a rapid and sustained between-group difference in SBP,” Prof. Cai pointed out. Over a median follow-up of 3.34 years, the event rate for the primary outcome was 3.5% on intensive treatment and 4.6% on standard therapy. Intensive treatment reduced the likelihood of primary outcome by 26% (HR 0.74; 95% CI 0.60–0.92; P=0.007). Prof. Cai highlighted that the intensive BP lowering approach provided a significant 33% reduction in stroke and acute coronary syndrome, 28% in major adverse cardiac events, and 73% reduction in heart failure (see Figure). However, no significant decrease was seen in all-cause mortality, atrial fibrillation, or coronary revascularisation. “The beneficial effects of the intensive treatment were consistent across our prespecified subgroup analysis, including age older than 70 or not, sex, baseline SBP levels, previous diabetes and 10-year Framingham risk score,” said Prof. Cai.
Figure: Intensive blood pressure lowering is beneficial in various secondary outcomes. Modified from [1]

As for safety outcomes, there was a significant difference in the rate of hypotension events (3.4% intensive group vs 2.6% standard group; P=0.03), but none concerning dizziness, severe events such as syncopes or fractures, nor deterioration of renal function. “The STEP results support that the SBP target in older patients should be set lower than 130 mmHg for better CV benefits without increasing serious adverse events as well as renal injuries,” concluded Prof Cai.
- Cai J. STEP Study: Intensive vs. standard blood pressure control among older hypertensive patients. Hot Line Session, ESC Congress 2021, 27–30 August.
- Zhang W, et al. N Eng J Med 2021;Aug 30. DOI:10.1056/NEJMoa2111437.
- Willams B. STEP Study – Discussant review. Hot Line Session, ESC Congress 2021, 27–30 August.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD Next Article
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality »
« Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD Next Article
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality »
Table of Contents: ESC 2021
Featured articles
2021 ESC Clinical Practice Guidelines
2021 ESC Guidelines on Heart Failure
2021 ESC/EACTS Guidelines on Valvular Heart Disease
2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronisation Therapy
2021 ESC Guidelines on Cardiovascular Disease Prevention
Best of the Hotline Sessions
Empagliflozin: First drug with clear benefit in HFpEF patients
CardioMEMS: neutral outcome but possible benefit prior to COVID-19
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality
Older hypertensive patients benefit from intensive blood pressure control
Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD
Late-Breaking Science in Heart Failure
Valsartan seems to attenuate hypertrophic cardiomyopathy progression
Dapagliflozin reduces incidence of sudden death in HFrEF patients
Late-Breaking Science in Hypertension
Smartphone app improves BP control independent of age, sex, and BMI
QUARTET demonstrates that simplicity is key in BP control
Salt substitutes: a successful strategy to improve blood pressure
Late-Breaking Science in Prevention
NATURE-PCSK9: Vaccine-like strategy successful in lowering CV events
Polypill: A successful tool in primary prevention
Important Results in Special Populations
VOYAGER PAD: Fragile or diabetic patients also benefit from rivaroxaban
COVID-19 and the Heart
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients
COVID-19: Thromboembolic risk reduction with therapeutic heparin dosing
Long COVID symptoms – Is ongoing cardiac damage the culprit?
ESC Spotlight of the Year 2021: Sudden Cardiac Death
Breathing problems: the most frequently reported symptom before cardiac arrest
Lay responders can improve survival in out-of-hospital cardiac arrest
Related Articles
October 26, 2021
QUARTET demonstrates that simplicity is key in BP control
October 26, 2021
Polypill: A successful tool in primary prevention
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

