The majority of sudden deaths are of cardiac aetiology and most of them are associated with arrhythmias [3]. Thus, the DAPA-HF (NCT03036124) trial evaluated dapagliflozin’s efficacy to prevent adverse outcomes of heart failure (HF) in patients with HF and reduced ejection fraction (HFrEF) [4]. The previously published main results showed a 26% risk reduction of the composite primary endpoint of cardiovascular death or worsening of HF. DAPA-HF included 4,744 patients with a left ventricular ejection fraction (LVEF) ≤40% and an NT-proBNP ≥600pg/mL who were in NYHA class II–IV. The mean age was 67 years, mean LVEF 31%, 45% suffered from diabetes, and 41% from chronic kidney disease. “Background HF therapy was very good,” Dr James Curtain (University of Glasgow, Scotland) stated referring to a high percentage of patients on renin-angiotensin-aldosterone inhibition, β-blocker, and mineralocorticoid receptor antagonists (MRA).
The primary outcome of this new analysis consisted of a composite of VA, resuscitated cardiac arrest, or sudden death. Furthermore, sensitivity analyses were performed, with composites that excluded non-sustained ventricular tachycardia or included only more serious VAs and predictors of the primary outcome were identified. Dr Curtain outlined that “315 patients or 6.6% of the total study cohort experienced a primary outcome event of which the majority, 64%, were adjudicated sudden death. VA accounted for 33% of the primary outcome events and there were 8 RCAs.”
Comparing patients without a primary outcome event with those who were subject to VA, resuscitated cardiac arrest, or sudden death, the latter were significantly more often men, had a history of prior VA, a lower LVEF, and had a lower eGFR. Also, primary outcome events were more likely to occur in those on a loop diuretic or having a defibrillating device.
Among the significant independent predictors of VA, resuscitated cardiac arrest, or sudden death were male sex, higher NTproBNP, history of VA or myocardial infarction. The risk of a primary outcome event was reduced by higher values of LVEF, systolic blood pressure, or serum sodium.
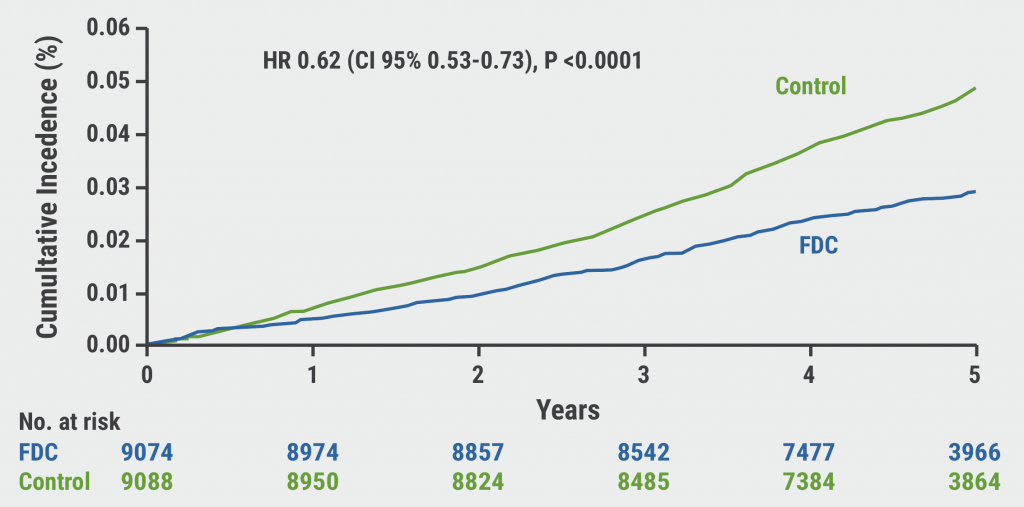
“Dapagliflozin compared with placebo reduced the incidence of the primary outcome VA, RCA, or sudden death by 21% with an HR of 0.79 and P-value of 0.037,” said Dr Curtain. He further elaborated that the results of the competing risk analysis including all-cause death were effectively the same with an incidence reduction by 20%. In his summary, Dr Curtain also pointed out that the effect of dapagliflozin was generally consistent across key subgroups and within several sensitivity analyses examining composites excluding non-sustained ventricular tachycardia or including only more serious VA.
- Curtain JP. DAPA-HF. Late-breaking science in heart failure, ESC Congress 2021, 27–30 August.
- Curtain JP, et al. Eur Heart J 2021;27 Aug. DOI:10.1093/eurheartj/ehab560.
- Kuriachan VP, et al. Curr Probl Cardiol. 2015;40(4):133–200.
- McMurray JJV, et al. N Engl J Med 2019;381:1995-2008.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Empagliflozin: First drug with clear benefit in HFpEF patients Next Article
Valsartan seems to attenuate hypertrophic cardiomyopathy progression »
« Empagliflozin: First drug with clear benefit in HFpEF patients Next Article
Valsartan seems to attenuate hypertrophic cardiomyopathy progression »
Table of Contents: ESC 2021
Featured articles
2021 ESC Clinical Practice Guidelines
2021 ESC Guidelines on Heart Failure
2021 ESC/EACTS Guidelines on Valvular Heart Disease
2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronisation Therapy
2021 ESC Guidelines on Cardiovascular Disease Prevention
Best of the Hotline Sessions
Empagliflozin: First drug with clear benefit in HFpEF patients
CardioMEMS: neutral outcome but possible benefit prior to COVID-19
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality
Older hypertensive patients benefit from intensive blood pressure control
Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD
Late-Breaking Science in Heart Failure
Valsartan seems to attenuate hypertrophic cardiomyopathy progression
Dapagliflozin reduces incidence of sudden death in HFrEF patients
Late-Breaking Science in Hypertension
Smartphone app improves BP control independent of age, sex, and BMI
QUARTET demonstrates that simplicity is key in BP control
Salt substitutes: a successful strategy to improve blood pressure
Late-Breaking Science in Prevention
NATURE-PCSK9: Vaccine-like strategy successful in lowering CV events
Polypill: A successful tool in primary prevention
Important Results in Special Populations
VOYAGER PAD: Fragile or diabetic patients also benefit from rivaroxaban
COVID-19 and the Heart
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients
COVID-19: Thromboembolic risk reduction with therapeutic heparin dosing
Long COVID symptoms – Is ongoing cardiac damage the culprit?
ESC Spotlight of the Year 2021: Sudden Cardiac Death
Breathing problems: the most frequently reported symptom before cardiac arrest
Lay responders can improve survival in out-of-hospital cardiac arrest
Related Articles
October 26, 2021
Polypill: A successful tool in primary prevention
October 26, 2021
2021 ESC/EACTS Guidelines on Valvular Heart Disease
October 26, 2021
Dapagliflozin reduces incidence of sudden death in HFrEF patients
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

