“Despite universal thromboprophylaxis with standard heparin, ‘breakthrough thrombotic events’ occur,” stated Prof. Alex Spyropoulos (Northwell Health, NY, USA). The HEP-COVID trial (NCT04401293) was designed to investigate thromboprophylaxis in high-risk, hospitalised patients with COVID-19, as the optimal regime for this population is still unknown. The study included 253 adult patients hospitalised with COVID-19 requiring oxygen supplementation, who had either D-dimer of 4x the upper normal limit or a sepsis-induced coagulopathy (SIC) score of ≥4. They were randomised to 2 subgroups of ICU and non-ICU treatment and further to subcutaneous enoxaparin 1mg/kg twice daily or standard-of-care /intermediate-dose heparin (SOC group) over 10+4 days or until discharge. Before discharge, a compression ultrasound was performed of the lower extremities. The primary composite efficacy endpoint consisted of venous thromboembolism (VTE), arterial thromboembolic events (ATE), and all-cause mortality after 30 days. The principal safety outcome was major bleeding.
The mean age of the modified intention-to-treat population was 66 years. Over 50% of participants were men, and the mean body mass index was around 30 kg/m2. Among the most frequent VTE risk factors were a history of VTE or cancer. The mean SIC score was 2.3 in both groups and D-dimer in the enoxaparin arm was 3,837 ng/mL versus 3,183 ng/mL in the SOC group. About one-third of the study subjects required ICU care and the mean length of in-patient care was close to 12 days.
The results demonstrated a relative risk (RR) of 0.68 (95% CI 0.49–0.96; P=0.0273) for the primary composite efficacy outcome with a 13.2 absolute risk reduction in favour of enoxaparin. Looking at ICU and non-ICU strata, the effect was driven by the non-ICU group with a RR of 0.46 (95% CI 0.27–0.81; P=0.0042), yet no significance in the ICU stratum (RR 0.92; 95% CI 0.62–1.39). The components VTE+ATE also revealed a significant risk reduction of 63% (P=0.0003), but all-cause mortality showed only a numerical between-group difference.
“The principal safety outcome of major bleeding occurred in 2 patients in the standard-dose group and 6 patients in the therapeutic-dose group with an incidence of 1.6% and 4.7%, and this was not statistically significant,” said Prof. Spyropoulos. In summary, he stressed that this trial was the first to show the superiority of a therapeutic dose of low-molecular-weight heparin over SOC thromboprophylaxis with overall low rates of bleeding in those selected for the trial.
- Spyropoulos AC. The HEP-COVID Trial. Latest Science in COVID-19, ESC Congress 2021, 27–30 August.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Long COVID symptoms – Is ongoing cardiac damage the culprit? Next Article
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients »
« Long COVID symptoms – Is ongoing cardiac damage the culprit? Next Article
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients »
Table of Contents: ESC 2021
Featured articles
2021 ESC Clinical Practice Guidelines
2021 ESC Guidelines on Heart Failure
2021 ESC/EACTS Guidelines on Valvular Heart Disease
2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronisation Therapy
2021 ESC Guidelines on Cardiovascular Disease Prevention
Best of the Hotline Sessions
Empagliflozin: First drug with clear benefit in HFpEF patients
CardioMEMS: neutral outcome but possible benefit prior to COVID-19
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality
Older hypertensive patients benefit from intensive blood pressure control
Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD
Late-Breaking Science in Heart Failure
Valsartan seems to attenuate hypertrophic cardiomyopathy progression
Dapagliflozin reduces incidence of sudden death in HFrEF patients
Late-Breaking Science in Hypertension
Smartphone app improves BP control independent of age, sex, and BMI
QUARTET demonstrates that simplicity is key in BP control
Salt substitutes: a successful strategy to improve blood pressure
Late-Breaking Science in Prevention
NATURE-PCSK9: Vaccine-like strategy successful in lowering CV events
Polypill: A successful tool in primary prevention
Important Results in Special Populations
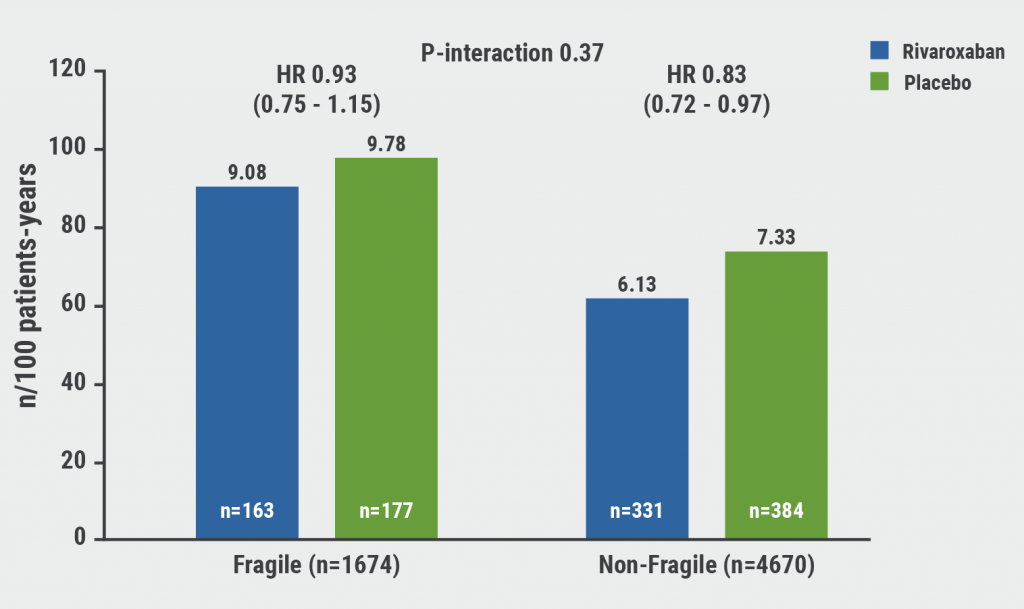
VOYAGER PAD: Fragile or diabetic patients also benefit from rivaroxaban
COVID-19 and the Heart
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients
COVID-19: Thromboembolic risk reduction with therapeutic heparin dosing
Long COVID symptoms – Is ongoing cardiac damage the culprit?
ESC Spotlight of the Year 2021: Sudden Cardiac Death
Breathing problems: the most frequently reported symptom before cardiac arrest
Lay responders can improve survival in out-of-hospital cardiac arrest
Related Articles
October 26, 2021
NATURE-PCSK9: Vaccine-like strategy successful in lowering CV events

September 14, 2021
ESC 2021 Highlights Podcast
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

