Although large studies in patients with diabetes have identified agents that lower major adverse cardiovascular event (MACE) rates, certain agents increase rates of lower extremity amputation (LEA). Especially patients with peripheral artery disease run a risk, as they have a greater incidence of diabetes and risk for lower extremity amputation.
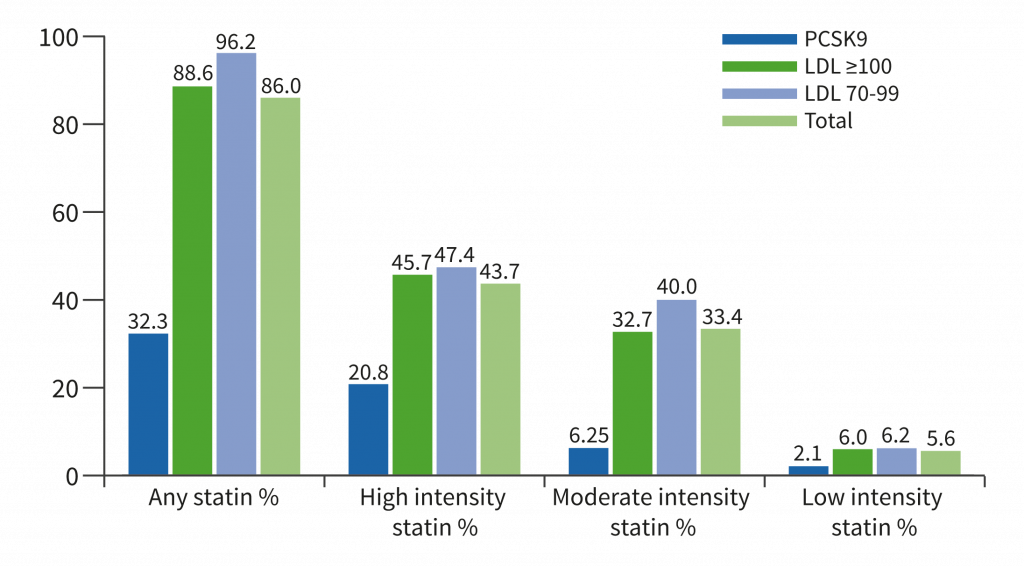
The EXSCEL study tested the effects of the GLP-1 agonist exenatide vs placebo on the rates of the primary composite MACE endpoint (i.e. CV death, myocardial infarction, or stroke) and a post-hoc analysis assessed the association of PAD with rates of MACE, LEA, and the effects of exenatide vs placebo in patients with and without PAD. The 2,800 enrolled PAD patients were numerically less likely to be on statin (65.8% vs 75.3%), betablockers (45.4% vs 58.1%), ACE inhibitor (45.2% vs 49.5%), and aspirin (57.3% vs 65%) compared with those without PAD. No difference was observed in rates of MACE in patients with or without PAD (HR adjusted 1.07; 95% CI, 0.95-1.20; P=0.29). However, patients with PAD had higher rates of all-cause mortality (HR adjusted 1.39; 95% CI, 1.21-1.61; P<0.001), and higher rates of lower limb events (HR adjusted 4.99; 95% CI, 4.15-5.99; P <0.001). The effect of exenatide vs placebo on MACE events in the PAD population (HR 0.85; 95% CI, 0.69-1.04) was similar to the effect in the no PAD population (HR 0.94; 95% CI, 0.84-1.04; Interaction P=0.42). The effect of exenatide vs placebo on lower limb events in the PAD population (HR 0.83; 95% CI, 0.66-1.04) was similar to the effect in the no PAD population (HR 0.96; 95% CI, 0.74-1.24; P=0.4). However, the trial was not designed or powered to observe a difference in lower extremity events.
The researchers concluded that PAD patients were less likely to be on optimal medical therapy for secondary prevention of CV disease, specifically statins, beta-blockers, ACE inhibitors, and aspirin. PAD patients had similar adjusted rates of MACE when compared with patients without PAD, yet they had higher rates of CV and all-cause mortality, and higher adverse lower limb events including LEA and limb revascularisation. Exenatide was not associated with LEA in patients with diabetes with and without baseline PAD. However, dedicated trials in PAD powered for limb outcomes are necessary to definitively determine the benefits of GLP1 agonists in this population.
1. Badjatiya A, et al. Abstract 1007-03. ACC 2019, 16-18 March, New Orleans, USA.
Posted on
Previous Article
« Lower rates stroke/SE with DOACs in frail non-valvular AF patients Next Article
Venetoclax-obinutuzumab combination elicits high response rates in CLL »
« Lower rates stroke/SE with DOACs in frail non-valvular AF patients Next Article
Venetoclax-obinutuzumab combination elicits high response rates in CLL »
Table of Contents: ACC 2019
Featured articles
Acute and Stable Ischaemic Heart Disease
Arrhythmias and Clinical Electrophysiology
Substantial impact of temporary interruptions of warfarin versus DOAC
Smartwatch can detect atrial fibrillation with high degree of accuracy
Congenital Heart Disease
Heart Failure and Cardiomyopathies
Frequent use of beta-blocker after HFpEF hospitalisations in elderly patients without compelling indications
High 5-year survival rates for older HF patients without initial severe comorbidity
Pulmonary Arterial Hypertension and Venous Thromboembolism
Interventional Cardiology
Vascular Medicine
Lower rates stroke/SE with DOACs in frail non-valvular AF patients
Similar rates of stroke/SE associated with DOAC vs warfarin use in obese non-valvular AF patients: Results from an observational registry
Convincing evidence of the role of icosapent in reducing subsequent CV events
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy