https://doi.org/10.55788/f538e95e
Presented by Prof. Alan Tita (University of Alabama, AL, USA), the Chronic Hypertension and Pregnancy (CHAP) trial (NCT02299414) aimed to assess the safety and efficacy of avoiding adverse pregnancy outcomes by treating pregnant women with mild chronic hypertension [1]. Prof. Tita pointed out that this is the largest, most diverse study conducted in pregnant women to date to address this major clinical question that has been debated for decades. The results were published simultaneously in the New England Journal of Medicine [2].
Enrolled were 2,408 women pregnant with a single foetus at <23 weeks of gestation. They were randomised to receive either antihypertensive treatments recommended for use in pregnancy (treatment group) or no treatment except in the case of severe hypertension (i.e. systolic pressure ≥160 mmHg or diastolic pressure ≥105 mmHg; control group). The primary efficacy endpoint was a composite of preeclampsia with severe features, medically indicated preterm birth <35 weeks gestation, placental abruption, or foetal/neonatal death. The safety endpoint was birth weight <10th percentile for gestational age.
Both the efficacy and safety endpoints were met. In the treatment group, 30.2% of women experienced an efficacy primary-outcome event, as opposed to 37% of pregnancies in the control group (HR 0.82; 95% CI 0.74–0.92; P<0.001). Importantly, this benefit was not coupled with a negative impact on gestational-age birth weights; the incidence of <10th percentile-for-gestational-age birth weights was 11.2% for the treatment group compared with 10.4% for the control group [risk ratio of 1.04, not significant]. The treatment group also had a modestly reduced incidence of serious maternal complications (2.1% and 2.8%, respectively; risk ratio 0.75; 95% CI 0.45–1.26) and severe neonatal complications (2.0% and 2.6%, respectively; risk ratio 0.77; 95% CI 0.45–1.30). Furthermore, the incidence of any preeclampsia favoured the treatment group at 24.4% and 31.1%, respectively (risk ratio 0.79; 95% CI 0.69–0.89), and the incidence of preterm birth was 27.5% and 31.4%, respectively (risk ratio 0.87; 95% CI 0.77– 0.99).
The take-home message from this trial is that treating pregnant women with mild chronic hypertension produces better pregnancy outcomes than a strategy of reserving treatment only for severe hypertension, with no increased risk of low foetal weight.
- Tita AT, et al. Antihypertensive Therapy For Mild Chronic Hypertension and Pregnancy Outcomes: A Pragmatic Multicenter RCT. Abstract 402–15, ACC 2022, 2–4 April, Washington DC, USA.
- Tita AT, et al. N Engl J Med 2022; 386:1781-1792.
Copyright ©2022 Medicom Medical Publishers
Posted on
Previous Article
« New VOYAGER PAD data: Should patients with both PAD and CKD get rivaroxaban? Next Article
POISE-3: Tranexamic acid for non-cardiac surgery »
« New VOYAGER PAD data: Should patients with both PAD and CKD get rivaroxaban? Next Article
POISE-3: Tranexamic acid for non-cardiac surgery »
Table of Contents: ACC 2022
Featured articles
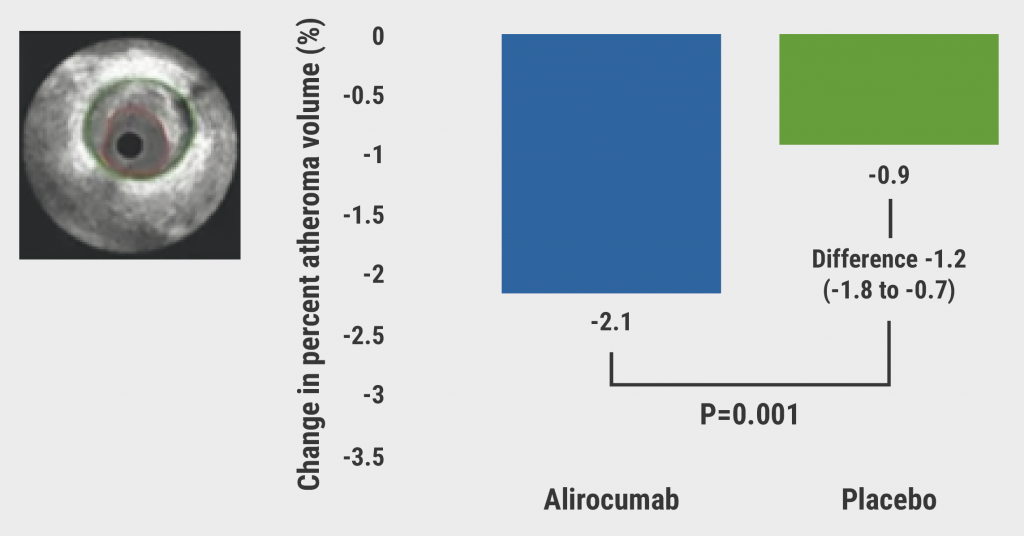
Alirocumab significantly reduces high-risk coronary plaques
Highlighted Original Research
POISE-3: Tranexamic acid for non-cardiac surgery
Treating chronic mild hypertension during pregnancy leads to better outcomes
New VOYAGER PAD data: Should patients with both PAD and CKD get rivaroxaban?
Alirocumab significantly reduces high-risk coronary plaques
Aggressive warming during non-cardiac surgery does not improve outcomes
Heart Failure and Cardiomyopathy
DIAMOND trial: Patiromer lowers risk of severe hyperkalaemia
Replacing septal reduction therapy with mavacamten for HCM
Omecamtiv mecarbil does not impact exercise capacity of patients with HFrEF
Symptomatic obstructive hypertrophic cardiomyopathy: long-term mavacamten control
Interventional and Structural Cardiology
COMPLETE revascularisation improves angina-related QoL
Plot twist for negative FAME 3 results: early QoL benefits of PCI
1-year CLASP TR results support tricuspid regurgitation repair
Head-to-head: post-TAVR edoxaban not better than DAPT
Chocolate Touch vs Lutonix catheters
No FLAVOUR difference between FFR and IVUS for PCI guidance
Myocardial Infarction
Low-resource countries benefit from global STEMI initiative
Sodium thiosulfate ineffective at cardiac protection
ICM-guided management did not improve MACE after MI
Prevention
PACIFIC-AF: Low bleeding rates for asundexian in atrial fibrillation
RCT-IVVE trial: Do HF patients benefit from annual flu shots?
TRANSLATE-TIMI 70: Primary endpoint met but safety concerns for vupanorsen
Lipoprotein(a) slashed by 98% in APOLLO trial
Dietary intervention from your supermarket
Related Articles
June 15, 2022
Surprise outcome for SODIUM-HF
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

