The current decision-making tree for surgical approaches in PD (see Figure) was presented by Dr Juan Ignacio Martínez-Salamanca (University Hospital Puerta de Hierro Majadahonda, Spain) [1,2]. Surgery indications are stable disease for at least 6 months, compromised ability to have coitus, extensive plaque calcification which may or may not respond to collagenase, failed conservative treatment, and a strong desire of the patient for complete resolution of the curvature [1].
Figure: Decision-making tree for PD management, including surgical and medical approaches. Based on the EAU Guidelines [2]
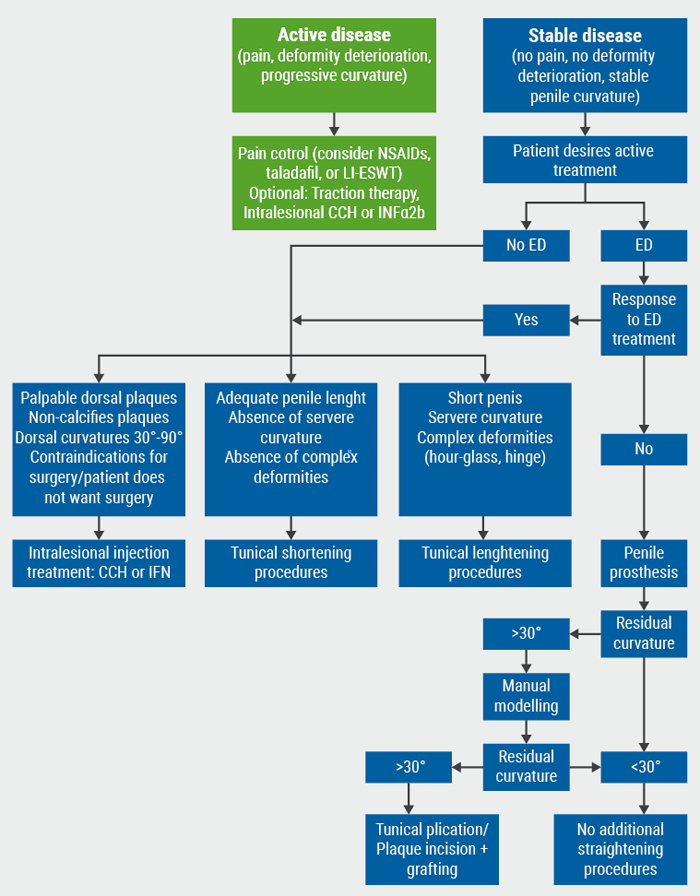
PD, Peyronie’s disease; ED, erectile dysfunction; NSAIDs, non-steroidal anti-inflammatory drugs; LI-ESWT, low-intensity extracorporeal shock waves therapy; CCH, collagenase Clostridium histolyticum; IFN, interferon.
Figure adapted from the EAU guidelines 2020.
The outcomes of tunical shortening procedures indicate that significant shortening occurs in less than 10% of individuals, although any amount of shortening occurs in 30-40% of patients. However, outcomes are good, with very low rates of de novo ED, as well as low penile hypoaesthesia rates. High satisfaction rates are reported. On the other hand, tunical lengthening procedures have a 90% success rate, although patients should be advised that some shortening could happen. However, de novo ED was high, up to 20-25% post procedure.
The recommendations, as listed by Dr Martínez-Salamanca, are [2]:
- Perform surgery only when PD has been stable for at least 3 months without pain or deterioration of the deformity;
- Prior to surgery, assess penile length, curvature severity, erectile function, and patient expectations;
- Use tunical shortening procedures as the first treatment option for congenital penile curvature or for PD with adequate penile length and rigidity, non-severe curvature, and absence of complex deformities. The type of procedure used is dependent on surgeon’s and patient's preference;
- Use tunical lengthening procedures for patients with PD and normal erectile function without adequate penile length, severe curvature, or presence of complex deformities such as hourglass or hinge shapes;
- The type of graft used is dependent on the surgeon and patient factors, no graft has proven superior;
- Do not use synthetic grafts in PD reconstructive surgery;
- Use sliding techniques with great caution as there is a significant risk of life-changing complications such as glans necrosis;
- Use penile prosthesis implantation with or without any additional procedures such as modelling, plication, incision, or excision with or without grafting in PD patients with ED not responding to pharmacotherapy.
Dr Martínez-Salamanca ended with take-home messages: (1) try to individualise each patient, to form an approach in line with the guidelines; (2) engage in an extensive discussion with your patient before surgery, balancing the patient’s expectations against real outcomes and the practitioner’s own experience; (3) be certain the surgeon and entire surgical team is fully trained and skilled, even to fix major complications. However, should complications occur, keep the patient updated and discuss all options openly.
- Martínez-Salamanca JI, et al. EAU20 Virtual Congress, 17-26 July 2020.
- EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam 2020. ISBN 978-94-92671-07-3.
Posted on
Previous Article
« Infertility and testis cancer risk: causal or association? Next Article
Unrecognised role of iron in neutrophil differentiation »
« Infertility and testis cancer risk: causal or association? Next Article
Unrecognised role of iron in neutrophil differentiation »
Table of Contents: EAU 2020
Featured articles
Surgical Techniques and Safety
The new adjustable artificial sphincter victo: Surgical technique and results after a follow-up of more than one year
New urosepsis data from the SERPENS study
Stones
Intra-operative cone-beam computed tomography for detecting residual stones in percutaneous nephrolithotomy
Pressure and temperature: do high-power lasers pose a threat?
Radiation stewardship for patient and endourologist
New lithotripter data: improved stone clearance
Renal Cancer
Beyond the limits of ultrasound: Three dimensional augmented reality robot assisted partial nephrectomy (3D AR-RAPN) for complex renal masses
Imaging guided surgery with augmented reality for robotic partial nephrectomy
KEYNOTE-426: no QoL differences pembrolizumab + axitinib versus sunitinib
Debate: upfront cytoreductive nephrectomy or not?
Robotic-assisted partial nephrectomy: lower morbidity
Bladder Cancer
Reduced BCG frequency, faster NMIBC recurrence
Nadofaragene firadenovec effective in BCG-unresponsive papillary NMIBC
Understanding MIBC biology for novel treatment options
Prostate Cancer & Imaging
Transperineal laser ablation of prostate
Prostatectomy: R-LRPE better than LRPE for continence
PSMA PET-CT staging is 27% more accurate
Docetaxel + hormonal therapy: improved prostate cancer PFS
ARAMIS subgroup analysis: darolutamide benefits across PSADT groups
Large patient-driven survey reveals QoL issues after prostate cancer treatment
Targeting steroid sulphatase in resistant prostate cancer cells
Good tolerance of post-RP radiotherapy ± short-term ADT
BPH & LUTS
Minimizing post-operative stress urinary incontinence after HoLEP: Our preliminary experience and short-term results of ‘’En Bloc’’ technique with early apical release
LUTS 2-year outcomes: aquablation versus TURP
HoLEP versus PVP in prospective randomised trial
Testis Cancer & Andrology
Peyronie’s disease: surgical options
Infertility and testis cancer risk: causal or association?
32% more men complain of reduced sex drive in 2019 versus 2009
Related Articles
July 22, 2022
Prostate cancer treatments reduce quality of life
August 21, 2020
PSMA PET-CT staging is 27% more accurate
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

