Tapering conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) or anti-tumour necrosis factor (TNF) showed no significant differences in flare ratios, disease activity, functional ability, and quality of life (QoL) between both tapering strategies during the first 12 months of follow-up. Early detection of RA, early initiation of ‘intensive’ therapy, and a treat-to-target (T2T) approach have led to substantial improvements in clinical and radiographic outcomes in RA over the last two decades. This has resulted in 50% to 60% of early RA patients achieving sustained remission during the first year of follow-up. Although current guidelines recommend to consider tapering treatment, an optimal approach to gradually de-escalate csDMARDs or bDMARDs is still lacking substantial evidence.
Van Mulligen et al. aimed to evaluate the effectiveness of two tapering strategies: gradual tapering of csDMARDs and TNF therapy during one year of follow-up.[8] This study was set up as a multicentre, single-blinded, randomised, controlled trial. Eligible patients were adults with RA <10 years (2010 criteria) who were in sustained remission for at least 3 consecutive months (defined as a disease activity score (DAS) ≤2.4 and a swollen joint count (SJC) ≤1), which was achieved with csDMARDs plus a TNF blocker combination therapy. Patients were randomised into gradual tapering csDMARDs followed by the TNF blocker or vice versa. Medication was tapered in three steps over the course of 6 months. Gradual tapering was done by cutting the dosage into half, a quarter, and thereafter it was stopped. The primary outcome for the clinical effectiveness was disease flare defined as DAS44 >2.4 and/or SJC >1. Secondary outcomes were QoL and functional ability.
A total of 189 patients were randomly assigned to tapering csDMARDs (n=94) or tapering anti-TNF agents (n=95). The majority of patients were female (71% in the csDMARDs tapering group, and 61% in the anti-TNF tapering group) with mean age of approximately 56 years. No significant difference in flare ratio was found; the cumulative flare ratio in the csDMARD and anti-TNF tapering group was 35% and 45%, respectively, with the biggest difference in increased cumulative flair ratio between the groups in the last 3 months. A longer extension study is needed to see if these results are sustainable in the long term, as everyone might eventually flare. The tapering status at 12 months revealed that 68% of those tapering csDMARDs had completely withdrawn their medication vs 51% for those tapering anti-TNF. Seven percent of patients tapering csDMARDs were at a quarter of the original dose (vs 20%), and 15% were at half of the original dose (vs 11%). Finally, 9% of csDMARDs tapering patients were (again) at the original dose vs 18% of those on anti-TNF (see Figure).
Figure: Tapering status at 12 months [8]
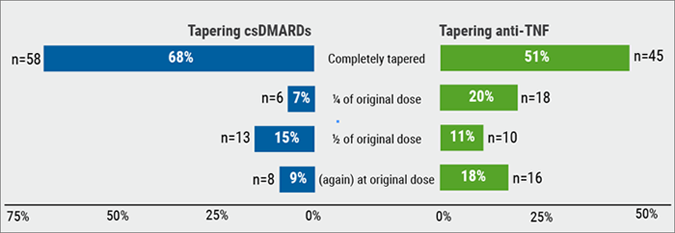
Furthermore, no difference in DAS was observed between groups, or in patient-reported outcomes (PROs). Based on these outcomes, Dr Van Mulligen (Erasmus MC, the Netherlands) pleaded to taper medication in RA patients who are in sustained remission with a preference to taper anti-TNF over cSDMARDs, but also taking into account the risk of a disease flare and considering the wishes of the patient with regard to therapy.[8]
- Van Mulligen E, et al. Abstract OP0113. EULAR 2018.
Posted on
Previous Article
« miRNA-146A plays key role in bone metabolism and osteoporosis Next Article
Glucosepane is a new biomarker for the severity of osteoarthritis »
« miRNA-146A plays key role in bone metabolism and osteoporosis Next Article
Glucosepane is a new biomarker for the severity of osteoarthritis »
Table of Contents: EULAR 2018
Featured articles
Rheumatoid Arthritis
Switching to biosimilar bDMARDs is safe and efficacious
No significant differences when tapering TNF blockers versus csDMARDs
Confirmation of long-term safety profile adalimumab across indications
Ankylosing Spondylitis
Clinical effect of vedolizumab on articular manifestations spondyloarthritis associated with IBD
Synergistic effect NSAIDs plus TNFi in slowing radiographic progression in ankylosing spondylitis patients
Osteoporosis and Osteoarthritis
Systemic Sclerosis and Systemic Lupus Erythematosus
Promising results rituximab in systemic sclerosis, and systemic lupus erythematosus classification criteria
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy