Allogeneic haematopoietic stem cell transplant (HSCT) recipients are at increased risk of severe RSV infection, so identifying patients at risk can be helpful in guiding treatment. Until new treatments are being approved, ribavirin is the only currently available treatment option. Two clinical scores were previously considered to predict the risk of progression to LRTI and death: the Immunodeficiency Scoring Index (ISI) from 2014 and the Severe Immuno-Deficiency (SID) score from 2008 (see Table) [1,2]. Current guidelines recommend to use ISI or SID scores to advise for treatment of RSV infection.
Table: Prognostic scoring systems: ISI and SID scores [1,2]
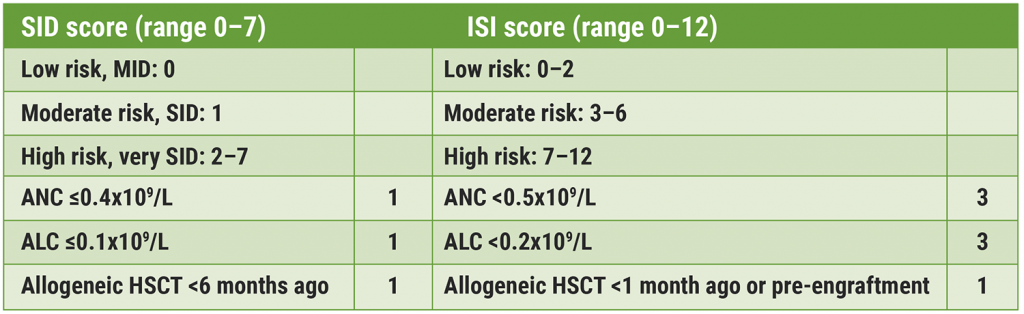
ALC, absolute lymphocyte count; ANC, absolute neutrophil count; GVHD, graft-versus-host disease; HSCT, haematopoietic stem cell transplantation; ISI, immunodeficiency scoring index; MID, moderate immune-deficiency; SID, severe immune-deficiency
The aim of the current study was to assess the prognostic value of the ISI and SID score using a retrospective multicentre cohort of allogeneic HSCT recipients [3,4]. Both adult and paediatric allogeneic HSCT recipients diagnosed with an RSV infection between 2010–2019 were included in 5 hospitals in France. Patients were stratified into 3 risk groups according to their (retrospective) ISI or SID score. Endpoints were overall survival (OS), RSV-attributable mortality, and progression from upper respiratory tract infection (URTI) to LRTI.
Of 147 patients that were electable for the study, 94 (64%) were initially diagnosed with URTI and 53 (36%) with LRTI. At day 90, 14 patients died with an estimated survival rate of 91%. Cumulative incidence of LRTI after URTI at day 60 was 14%. The stratification of disease severity according to either ISI or SID score did not demonstrate any difference in either overall mortality or RSV-attributable mortality. However, the ISI score could predict the risk for progression from URTI to LRTI (P=0.0008).
In short, data from this multicentre retrospective study of allogeneic HSCT recipients with PCR-confirmed RSV infection showed that neither the ISI nor the SID score demonstrated prognostic value for mortality, but the ISI score allowed for the prediction of progression to LRTI. More research is needed for future implementation of the scores.
- Khanna N, et al. Clin Infect Dis. 2008 Feb 1;46(3):402-12.
- Shah DP, et al. Blood. 2014;123(21):3263–8.
- Houist A, et al. Evaluation of two prognostic scoring systems for respiratory syncytial virus infection in a French multicentre cohort of allogeneic hematopoietic stem cell transplant recipients. Abstract 1893. ERS 2021, 5–8 September.
- Houist A, et al. Bone Marrow Transplant. 2021 Sep 21;1-10.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Livestock farming affected the airway microbiome of COPD patients Next Article
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma »
« Livestock farming affected the airway microbiome of COPD patients Next Article
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma »
Table of Contents: ERS 2021
Featured articles
Letter from the Editor
COVID-19 Research: Looking Back and Moving Forward
Higher inflammation markers in COVID-19 patients with a first negative PCR test
Persistent fatigue following COVID-19
Risk of COVID-19-related morbidity and mortality in young and middle-aged adults
Respiratory Viral Infections: Insights from Recent Studies
Rhinovirus bronchiolitis increased risk of recurrent wheezing and asthma
COPD: Evidence Update
Livestock farming affected the airway microbiome of COPD patients
Reduction of COPD severe acute exacerbations by candidate vaccine
Paediatrics and Vaccinology
Better lung function in children with a healthy diet
Need for validated severity score in the assessment of bronchiolitis
Increased impact of air pollution on lung function in preterm infants
Pearls in Asthma Research
Biomarkers do not discriminate severe from severe uncontrolled asthma
Increased blood neutrophiles in patients with obesity and asthma
Blood inflammatory phenotypes associated with clinical symptoms of asthma
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com