It is known that IBD patients have an increased colorectal cancer (CRC) risk, which is further increased following colonic low-grade dysplasia (LGD).
Endoscopic surveillance programmes aim to reduce CRC risk by detecting and removing pre-cancerous lesions such as LGD. Long-term risk of high-grade dysplasia (HGD) or CRC after LGD is relatively unknown, as most available studies are small and cover short follow-up periods.
A Dutch study presented results from a nationwide cohort of IBD patients with LGD. Long-term cumulative incidence of advanced neoplasia (HGD and/or CRC) was determined to be 21.9% after 15 years [1]. Meanwhile, older age at LGD, longer IBD duration before LGD, and male gender were recognised as independent risk factors for advanced neoplasia development. All IBD patients presenting with LGD between 1991 and 2005 in the Netherlands were identified using the Dutch National Pathology Registry. Follow-up data were collected until January 2016.
A total of 2,738 patients with colonic LGD were identified. Median follow-up was 9.5 years after initial LGD diagnosis (72.4% UC, 19.8% CD, and 7.9% indeterminate colitis). Colectomy was performed in 15.5% of patients. Advanced neoplasia was detected in 14.4% of patients, including 240 patients with CRC. The cumulative incidence of advanced neoplasia was 3.5%, 9.1%, 14.4%, 21.9%, and 29.9% after 1, 5, 10, 15, and 20 years, respectively (see Figure).
Figure: Cumulative incidence of HGD/CRC following LGD in IBD [1]
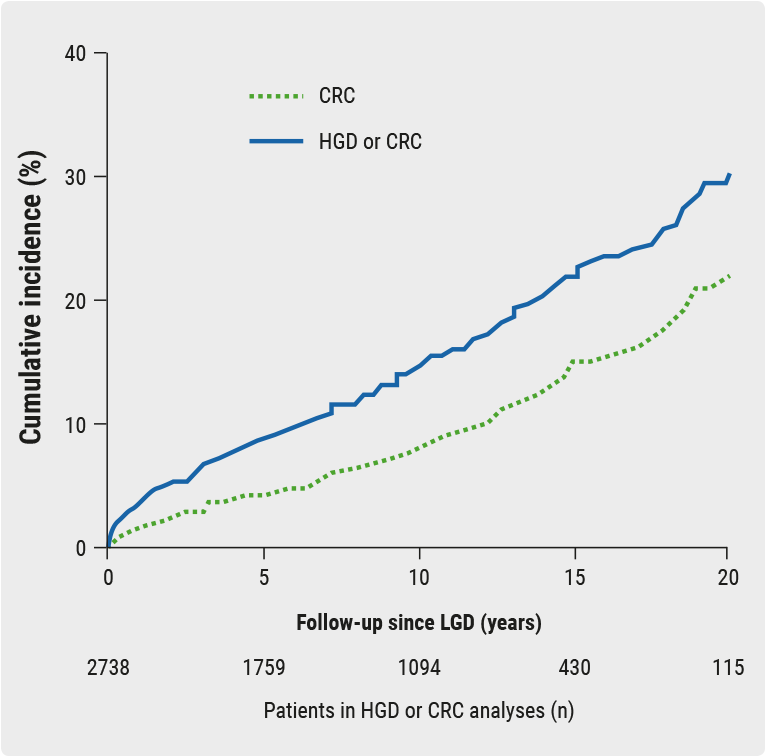
Median time to developing advanced neoplasia after LGD was 4.7 years. Multivariable analysis identified independent risk factors for advanced neoplasia following LGD. These included higher age (>55 years) at initial LGD (HR 1.87; 95% CI 1.53-2.30) and IBD duration >5 years before LGD (HR 1.46; 95% CI 1.13-1.90). In addition, male gender (HR 1.37; 95% CI 1.10-1.71) was also a risk. Findings of this study may aid in risk stratification for endoscopic surveillance after LGD in patients with IBD.
- de Jong MJ, et al. OP036. ECCO 2018.
Posted on
Previous Article
« Vedolizumab in anti-TNF-naïve IBD patients and safety profile Next Article
Combining new drugs with different mechanisms »
« Vedolizumab in anti-TNF-naïve IBD patients and safety profile Next Article
Combining new drugs with different mechanisms »
Table of Contents: ECCO 2018
Featured articles
IBD diagnostics
IBD disease patterns and genetics
Novel treatment strategies
Efficacy and safety of biologics
Oncology in IBD
Surgery for IBD
Related Articles
May 28, 2018
Long-term safety profile of adalimumab

© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

