Migraine headaches and dry eye disease are important health concerns, both being highly prevalent, debilitating, and known to decrease quality of life [2]. Hence, their association warrants further exploration.
The relation between migraine and dry eye disease is bidirectional and has been tested both ways, Dr Bithi Chowdhury (Hindu Rao Hospital and MDMC Medical College, India) mentioned. A previous Korean population-based study found dry eye disease to be significantly more prevalent in patients with migraine compared with controls (14.4% vs 8.2%; P=0.0001). Moreover, the presence of migraine was found to increase the odds of a dry eye diagnosis 1.6-fold and the odds of dry eye symptoms 1.3-fold [3]. Similarly, more patients with migraine tend to have a dry eye diagnosis than without migraine [4], in patients with migraine visual function and overall quality of life is correlated with dry eye symptoms [5], and the presence of a dry eye diagnosis increases the odds of a migraine diagnosis [6].
The current cross-sectional, observational, hospital-based study from India included 60 consecutive preventive-drug-naïve patients with migraine and 60 controls (i.e., patients presenting with refractive error without any migraine), aged 18–65 years [1]. Patients with comorbidities that can cause dry eye disease were excluded. Severe dry eye disease was diagnosed using the ODISSEY algorithm. Only the severely affected eye was used for comparison.
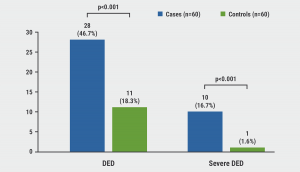
The mean tear break-up time (11.65 vs 14.30 seconds) and fluorescein scores (1.125 vs 0.692) were significantly worse in patients with migraine compared with controls (P=0.010). The prevalence of dry eye disease was found to be significantly higher in patients with migraine compared with controls (46.7% vs 18.3%; P<0.001). Moreover, severe dry eye disease was found to be significantly more prevalent in patients with migraine versus controls (16.7% vs 1.6%, P<0.001; see Figure).
Figure: Prevalence of (severe) dry eye disease [1]
Among patients with migraine, only mean pain severity was significantly associated with the presence of dry eye disease. Patients with migraine with severe dry eye disease had a higher frequency and severity of headache attacks. Together, these results suggest an association between dry eye and migraine.
- Chowdhury B, et al. Dry eye disease in migraine: A case control study. AL05, IHC 2021, 8–12 September.
- McDonald M, et al. Ocul Surf. 2016;14(2):144–67.
- Ozudogru S, et al. Headache. 2019;59(10):1714–21.
- Yang S, et al. Curr Eye Res. 2017;42(6):837–41.
- Ismail OM, et al. JAMA Ophthalmol. 2019;137(5):532–6.
- Wang TJ, et al. Acta Ophthalmol. 2012;90(7):663–8.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Voice change and throat swelling are cranial autonomic symptoms in primary headache Next Article
Predictors of health-related quality of life in cluster headache »
« Voice change and throat swelling are cranial autonomic symptoms in primary headache Next Article
Predictors of health-related quality of life in cluster headache »
Table of Contents: IHC 2021
Featured articles
Letter from the Editor
COVID-19
Telemedicine beneficial for headache care during the pandemic
Comparison of headaches after SARS-CoV-2 vaccination
Grey matter cortical changes in patients with persistent headache after COVID-19
Increased risk of cerebral venous thrombosis in COVID-19
Patient Perception and Symptoms
Predictors of health-related quality of life in cluster headache
Dry eye disease is more prevalent in migraine
Voice change and throat swelling are cranial autonomic symptoms in primary headache
Association between physical inactivity and headache disorders
Increased suicidal attempts and risks of ideation in medication-overuse headache
Cardioembolic Comorbidities
AI-enabled ECG algorithm predicts atrial fibrillation risk in migraine
Migraine may not be a risk factor for stroke
Imaging
Functional brainstem somatotopy of the trigeminal nerve during nociception
Morphological changes in cluster headache between attacks
Interictal pontine metabolism in migraine patients without aura
Genome-Wide Association Studies
Largest genome-wide association study of migraine to date
Robust evidence that cluster headache has a genetic basis
Pharmacological Treatment
Insights in drug-drug interactions facilitate rational polypharmacy
Rimegepant confers long-term improvements in MMDs
First real-world effectiveness data of erenumab is promising
Galcanezumab effective in patients with episodic or chronic cluster headache
Central effects and affected somatosensory processing with galcanezumab in migraine
Long-term safety and tolerability of atogepant in migraine
Non-Pharmacological Treatment
Occipital nerve stimulation effective and safe in chronic cluster headache
Related Articles
August 27, 2019
Factors influencing choice of prophylactic migraine therapy
November 8, 2021
Long-term safety and tolerability of atogepant in migraine
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

