Many observational studies have shown that complete revascularisation (CR; encompassing both ACR and ischaemic, or functional complete revascularisation [FCR]) following percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) procedures is associated with fewer subsequent major adverse cardiac events (MACE) than incomplete revascularisation (IR) [1,2]. However, this association is not always found, and few studies have adjusted for differences in baseline clinical and anatomic covariates [1,2]. Evidence was also lacking on the impact of CR on patients receiving an invasive versus a conservative management strategy. This was the motivation for a pre-planned sub-analysis of the ISCHEMIA trial (NCT01471522), which was presented by Dr Gregg Stone (Mount Sinai Medical Centre, NY, USA).
Previously published results from the ISCHEMIA trial (n=5,179) found no evidence that the use of an initially invasive strategy reduced the risk of ischaemic cardiovascular events or death from any cause when compared with an initially conservative strategy (optimal medical therapy alone) [3]. The current ISCHEMIA sub-study had 2 objectives: (1) to compare the outcomes of ACR and FCR with IR in patients who underwent an initially invasive strategy, and (2) to examine the impact that CR may have had in those patients who underwent an initially invasive strategy compared with an initially conservative strategy.
To satisfy the first objective, angiographic core laboratory assessments were conducted on 2,296 patients to determine the degree of completeness of revascularisation following PCI and CABG. Among patients in the invasive strategy arm, 1,802 had achieved ACR versus anatomic IR (a CR rate of 43.3%), and 1,743 had achieved FCR versus functional IR (a CR rate of 58.3%). In the ACR group, revascularisation had been achieved by PCI in 72.3%, CABG in 26.4%, and a hybrid approach in 1.3% of cases (see Figure 1). In the FCR group, revascularisation was achieved by PCI in 71.6%, CABG in 27.0%, and a hybrid approach in 1.4% of cases. Clinical predictors of completeness of revascularisation were anatomic, including the number of chronic total occlusions, the number of diseased vessels and lesions, and SYNTAX score. Multivariable analysis showed that CABG was associated with a higher rate of CR than PCI.
Figure 1: Completeness of revascularisation in patients using an invasive strategy [1]

ACR, anatomic complete revascularisation; CABG, coronary artery bypass graft; FCR, functional complete revascularisation; PCI, percutaneous coronary intervention.
Comparing the impact of complete versus incomplete revascularisation on the primary endpoint of cardiovascular death, myocardial infarction, hospitalisation for cardiac arrest, heart failure, or unstable angina, the adjusted hazard ratio in the ACR group was 0.79 (95% CI 0.55–1.15; P=0.22), while in the FCR group it was 0.96 (95% CI 0.68–1.34; P=0.80).
To fulfil the secondary objective, all 2,296 patients who had undergone an initially invasive strategy were compared with the 2,498 patients who had been treated conservatively, using an inverse probability weighted analysis. Overall rates of revascularisation were similar to those observed in the first group; 43.6% had achieved ACR, and 58.5% had achieved FCR (see Figure 2). Comparing primary outcomes in the ACR showed an overall 3.5% difference, favouring the invasively managed group over the conservatively managed group; this effect was somewhat smaller in the FCR group, showing an overall 2.3% difference, also favouring the invasively managed group. The overall results from the ISCHEMIA trial show a 2.5% difference, favouring the invasively managed group over the conservatively managed group.
Figure 2: Completeness of revascularisation in patients treated using an invasive strategy versus a conservative strategy [1]

ACR, anatomic complete revascularisation; CABG, coronary artery bypass graft; FCR, functional complete revascularisation; PCI, percutaneous coronary intervention.
The researchers cautioned that these results represent associations and not necessarily causality; however, they also concluded that these results suggest that in patients with chronic coronary syndrome, better outcomes may be achieved with an invasive approach over a conservative approach if ACR can be achieved. For this reason, the likelihood of safely achieving ACR should be considered when choosing the treatment strategy for patients in this population.
- Stone GW. Impact of completeness of revascularization on clinical outcomes in patients with stable ischaemic heart disease treated with an invasive versus conservative strategy: the ISCHAEMIA trial. ACC 2021 Scientific Session, 15–17 May 2021.
- Gaba P, et al. Nat Rev Cardiol. 2021;18:155–168.
- Maron DJ, et al. N Engl J Med 2020;382:1395–1407.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Letter from the Editor Next Article
Finerenone reduces the risk of AF onset in patients with CKD and diabetes »
« Letter from the Editor Next Article
Finerenone reduces the risk of AF onset in patients with CKD and diabetes »
Table of Contents: ACC 2021
Featured articles
Electrophysiology
Favourable outcomes with transcatheter atrial appendage occlusion
Etripamil nasal spray significantly improves PSVT-related symptoms
Ablation-based rhythm control as effective as rate control in AF and HF
Finerenone reduces the risk of AF onset in patients with CKD and diabetes
Heart Failure and Cardiomyopathy
PARADISE-MI: Sacubitril/valsartan not superior to ramipril in reducing HF events
Older adults with heart failure benefit from rehabilitation programme
Quality improvement intervention fails to improve care for patients with heart failure
Sacubitril/valsartan does not reduce NT-proBNP versus valsartan alone in HFrEF
Novel use of ivabradine in reversible cardiomyopathy
Mavacamten significantly improves QoL of patients with hypertrophic cardiomyopathy
Interventional and Structural Cardiology
Men and women benefit equally from early aspirin withdrawal following PCI
Similar outcomes with fractional flow reserve and angiography-guided revascularisation
TALOS-AMI: Exploring outcomes after switching to clopidogrel versus ticagrelor at 1 month from MI
Clopidogrel monotherapy associated with better net outcomes relative to aspirin monotherapy 6-18 months after PCI
Ischaemic Heart Disease
No difference in ischaemic risk or bleeding with low vs high-dose aspirin for secondary prevention: Lessons and questions from the ADAPTABLE trial
Rivaroxaban reduces total ischaemic events after peripheral artery revascularisation
Moderate hypothermia not superior to mild hypothermia following out-of-hospital cardiac arrest
Better outcomes with invasive strategy if anatomic complete revascularisation is possible
Prevention and Health Promotion
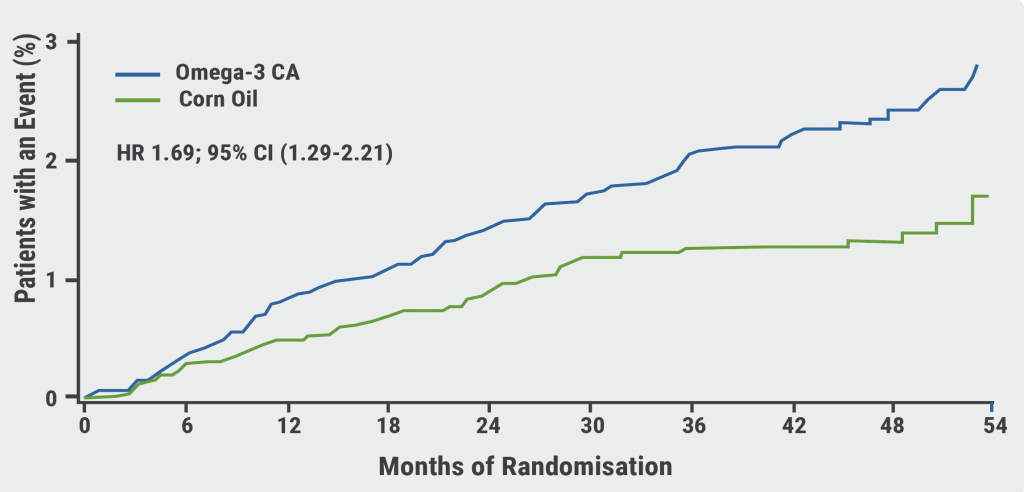
STRENGTH trial fails to demonstrate cardioprotective effect of omega-3 fatty acids
Evinacumab lowers triglyceride levels in severe hypertriglyceridaemia
Health equity and the role of the cardiologist: 7 priorities to consider
COVID-19
Dapagliflozin fails to show a significant protective effect in COVID-19
Therapeutic anticoagulation not superior to prophylactic anticoagulation in COVID-19
Atorvastatin does not reduce mortality in COVID-19
Valvular Heart Disease
Apixaban outcomes similar to current standard of care following TAVR
Preliminary results encouraging for EVOQUE tricuspid valve replacement
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com