The 10-year follow-up in the population-based NELSON trial showed that CT screening of high-risk men reduces lung cancer death rates by 26% (95% CI 9-41%). In a smaller subset of women, the reduction was even larger. Prof. Harry de Koning (Erasmus Medical Center, the Netherlands) presented the outcomes [8].
The NELSON trial is not the first large study to show a survival benefit with population-based lung cancer screening. The original landmark study, the National Lung Screening Trial (NLST), was conducted in the United States in 2011 and demonstrated a 20% relative reduction in lung cancer deaths for annual screening with low-dose CT over 3 years vs chest radiography [9].
The NELSON study, conducted in the Netherlands and Belgium, used nodule volume management for referral. It was designed to show a 25% reduction in lung cancer in males at the 10-year follow-up. The trial enrolled 15,822 subjects aged 50-74 years. In the overall cohort, the mean number of pack-years smoked was approximately 40 years.
Participants were randomised (1:1) to CT-screening at 1, 3, and 5.5 years, or no screening. Their records were linked to national registries with 100% coverage of cancer diagnosis, date of death, and cause of death. An expert panel blinded to study arm reviewed medical files on deceased lung cancer patients up to 2013; they subsequently used cause of death reported by Statistics Netherlands.
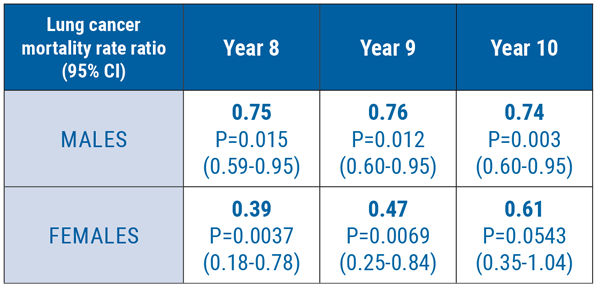
Follow-up through December 2015 comprised a minimum of 10 years follow-up of the 98.7% of patients who were still alive. Average CT screening compliance was 94%, which led to 29,736 scans. Additional scans within 2 months were performed on 9.1% of patients to estimate nodule volume doubling time. This led to an overall referral rate for suspicious nodule of 2.1%. In 9.3% of scans, results were indeterminate; 2.2% of scans were positive and lung cancer was detected in 0.9%. In these cases, 69% were detected at stage 1A or B. This was a much higher proportion of early-stage diagnoses compared with a cancer registry in the Netherlands. The positive predictive value of screening was 41% on a positive screen. This value was associated with a significant decrease in lung cancer mortality at 10 years in men (HR 0.74; P=0.003). The survival benefit was greater in women (HR 0.61; P=0.0543) as shown in the Figure. Surgery was 3 times more prevalent in a subset of CT-screened lung cancer patients compared with those in the control group (67.7% vs 24.5%; P<0.001). According to Prof. de Koning, these results should be used to inform and direct future CT screening around the world.
Figure: Lung cancer mortality rate ratio in the NELSON trial [8]
- De Koning HJ, et al. Abstract PL02.05. IASLC 19th WCLC. 23-26 September 2018, Toronto, Canada.
- National Lung Screening Trial Research Team. N Engl J Med 2011;365:395-409.
Posted on
Previous Article
« Crizotinib-treated ALK IHC-positive advanced NSCLC is associated with an unfavourable prognosis when FISH negative Next Article
Effects of dose modifications on safety and efficacy of dacomitinib for EGFR-mutant non-small-cell lung cancer »
« Crizotinib-treated ALK IHC-positive advanced NSCLC is associated with an unfavourable prognosis when FISH negative Next Article
Effects of dose modifications on safety and efficacy of dacomitinib for EGFR-mutant non-small-cell lung cancer »
Table of Contents: WCLC 2018
Featured articles
Interview with the IASCL President, Dr. Giorgio Scagliotti
Presidential Symposium – Top 5 abstracts
Durvalumab after chemoradiotherapy extends OS in stage 3, unresectable non-small-cell lung cancer
Potential for brigatinib as a first-line treatment option for ALK+ non-small-cell lung cancer
Benefits of chest CT screening
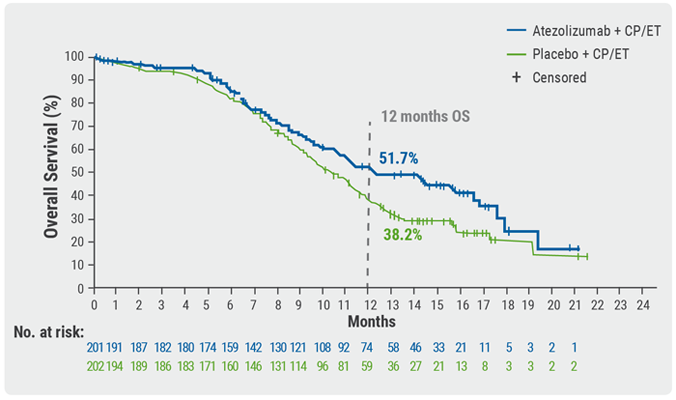
New standard of care in extensive-stage small-cell lung cancer
No progression-free survival benefit with nintedanib plus pemetrexed/cisplatin for malignant pleural mesothelioma of epithelial subtype
New Aspects of Immunotherapy
Next generation immunotherapy in non-small-cell lung cancer
Combination therapies: Where are we in 2018?
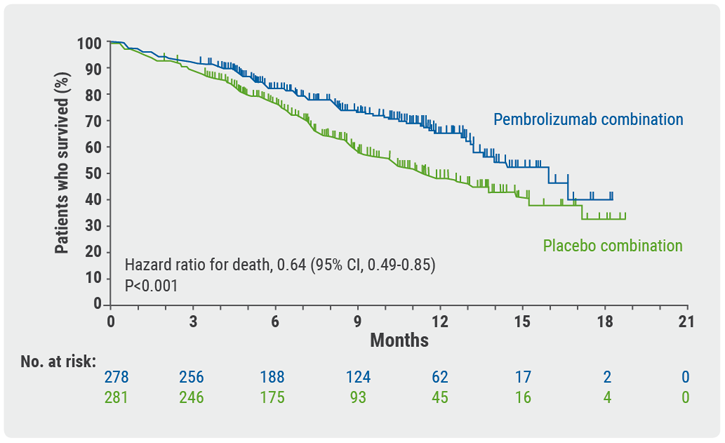
Choice of taxane and addition of pembrolizumab for metastatic squamous non-small-cell lung cancer
New Aspects of Targeted Therapy
PD-L1 expression in untreated EGFR-mutant non-small-cell lung cancer and response to osimertinib
Mesothelioma
Unmet needs in surgical management of malignant pleural mesothelioma
Advanced Non-small Cell Lung Cancer
Novel Therapies in ROS1 and EGFR
Advances in Small-cell and Neuroendocrine Tumours
Related Articles
November 21, 2018
New standard of care in extensive-stage small-cell lung cancer
November 21, 2018
Angiogenic and stromal biomarkers in malignant mesothelioma
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

