Prof. Usman Baber (Icahn School of Medicine at Mount Sinai, USA) provided the rationale behind this particular sub-analysis: “The basis for DAPT in ACS really comes from trials conducted almost 20 years ago showing that it is superior to aspirin,” but he noted that “one of the challenges we have with the provision of antiplatelet therapy right now is that a lot of patients who should probably be getting potent agents are not getting them due to concerns of bleeding” [1].
Of the 4,614 ACS patients enrolled in TWILIGHT, 2,494 had unstable angina and 2,120 had NSTEMI. Patients were randomised to drop aspirin after 3 months and continue ticagrelor monotherapy (n=2,273) or to continue with DAPT (n=2,341). Patient characteristics were similar in both groups; the mean age was 64 years, 35% had diabetes, and 61% had multivessel disease. There were, however, more smokers in the continued DAPT arm of the trial (26.6% vs 23.3%; P=0.02).
The primary endpoint at 1 year was Bleeding Academic Research Consortium (BARC) 2, 3, or 5. The results showed that the primary endpoint was met: bleeding was significantly lower in the ticagrelor monotherapy group compared with the arm that continued DAPT (3.6% vs 7.6%; HR 0.47; 95% CI 0.36-0.61; P<0.001). The 2 arms appeared similar for the secondary endpoint of all-cause death, MI, or stroke at 1 year (4.3% vs 4.4%; HR 0.97; 95% CI 0.74-1.28; P=0.84). Neither risk factors at presentation nor whether the patients had presented with unstable angina or NSTEMI made a difference. Prespecified ischaemic endpoints between the 2 arms were similar, including cardiovascular death, all-cause death, any MI, stroke, and stent thrombosis.
1. Baber U, et al. Ticagrelor with aspirin or alone in high-risk patients after coronary intervention for acute coronary syndrome. LBS04, AHA Scientific Sessions 2019, 14-18 November, Philadelphia, USA.
Posted on
Previous Article
« Icosapent ethyl plus statins reduces total plaque volume Next Article
Off-the-shelf natural killer cells »
« Icosapent ethyl plus statins reduces total plaque volume Next Article
Off-the-shelf natural killer cells »
Table of Contents: AHA 2019
Featured articles
New Approaches to CVD Risk Reduction
Phase 3 BETonMACE trial did not meet its primary endpoint
Inclisiran safely halves LDL-Cholesterol
Colchicine prevents cardiovascular events
Interventional Management for Acute Coronary Syndrome
Drop aspirin after 3 months in non-STEMI ACS patients on dual antiplatelet therapy
Immediate coronary angiography after cardiac arrest does not improve survival
Complete revascularisation for obstructive non-culprit lesions with vulnerable plaque
Colchicine: no difference in peri-procedural cardiovascular events 30 days post-PCI
Intra-aortic balloon pump better than Impella: new observational data
Results for the Ischemia Trials: To Intervene or Not to Intervene
ISCHEMIA trial: Invasive treatment only better for angina burden
Controversies in Contemporary Management of Aortic Stenosis
Full GALILEO results: Why did rivaroxaban fail after TAVR?
Balloon-expandable better than self-expanding transcatheter heart valves
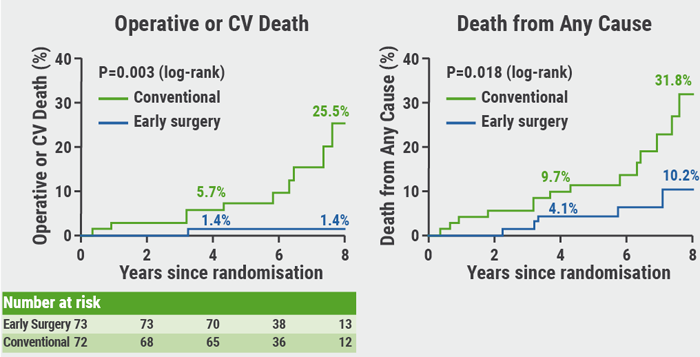
RECOVERY: Benefit of early surgery in asymptomatic severe aortic stenosis
Guidelines: Updates and Controversies
New guidelines on the prevention of cardiovascular conditions
Trials in Electrophysiology and Left Ventricular Function
RENAL-AF trial: Apixaban similar to warfarin
Apple Heart Study: Not just for atrial fibrillation
Early apixaban safe as secondary prevention of stroke from AF
Carvedilol does not improve exercise performance in Fontan patients
New Frontiers in Lipid Therapy
Icosapent ethyl plus statins reduces total plaque volume
ORION-9: Inclisiran RNAi halves LDL in familial hypercholesterolaemia patients
New RNAi therapies to reduce triglycerides: 2 studies show favourable results
Targeting LDL-C <70 mg/dL is better than 100 mg/dL after stroke
Challenges in Heart Failure Management
FUEL trial: Udenafil improves some exercise measurements in Fontan
DAPA-HF: Dapagliflozin also good for heart failure patients without diabetes, of any age, or any health status
PARAGON-HF: Benefits for women and lower ejection fraction
Related Articles
February 26, 2020
Balloon-expandable better than self-expanding transcatheter heart valves
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

