Dr Isabel Graupera (Institut d'Investigacions Biomediques August Pi I Sunyer, Barcelona, Spain) reported the positive results from the prespecified 18-month interim analysis of the phase 3, randomised, double-blind, placebo-controlled, multicentre study REGENERATE study of OCA in patients with liver fibrosis due to NASH [1], which was conducted to assess the effect of OCA on liver histology comparing baseline biopsies with biopsies taken at month 18. The intention-to-treat population for the interim analysis included 931 patients with stage 2 and 3 fibrosis (placebo, n=311; OCA 10 mg, n=312; OCA 25 mg, n=308). REGENERATE has completed target enrolment for the clinical outcomes cohort, with 2,480 adult NASH patients randomised, and will continue through clinical outcomes for verification and description of clinical benefit.
The fibrosis improvement endpoint was achieved by 37 (12%) patients in the placebo group, 55 (18%) in the OCA 10 mg group (P=0.045), and 71 (23%) in the OCA 25 mg group (P=0.0002). The NASH resolution endpoint was not met (8% of patients in the placebo group, 11% in the OCA 10 mg group [P=0.18], and 12% in the OCA 25 mg group [P=0.13])
The safety population of the interim analysis included 1,968 randomised patients who received at least one dose of study drug (OCA or placebo). Adverse events were generally mild to moderate in severity and the most common were consistent with the known profile of OCA. The frequency of serious adverse events was similar across treatment arms (11% in placebo, 11% in OCA 10 mg, and 14% in OCA 25 mg). The most common adverse event reported was dose-dependent pruritus (placebo, 19%; OCA 10 mg, 28%; OCA 25 mg, 51%). The large majority of pruritus events were mild to moderate.
Dr Graupera concluded, “The antifibrotic efficacy observed with just 18 months of OCA treatment in REGENERATE is particularly meaningful because fibrosis is the most important histological predictor of liver failure and death in patients with NASH.”
- Graupera I et al. UEG Week 2019, Abstract OP196.
Posted on
Previous Article
« Interim data on GOULASH-PLUS trial Next Article
Immunonutrition during neoadjuvant oesophagogastric cancer therapy: no benefit »
« Interim data on GOULASH-PLUS trial Next Article
Immunonutrition during neoadjuvant oesophagogastric cancer therapy: no benefit »
Table of Contents: UEGW 2019
Featured articles
Interview with UEG President Prof. Paul Fockens
Upper GI Disorders
Locally active corticosteroid promising in eosinophilic oesophagitis
First-in-human radiofrequency vapor ablation in Barrett’s oesophagus
Irritable Bowel Syndrome
Faecal microbiota transplantation is effective for irritable bowel syndrome
Human milk oligosaccharides improve IBS symptoms
Inflammatory Bowel Disease
Ustekinumab is safe and effective in ulcerative colitis: 2-year data
Decreased microvilli length in CD patients
Phase 2 data shows benefit for mirikizumab in CD patients
Subcutaneous ustekinumab as maintenance therapy in UC
First evidence of long-term efficacy of ABX464 in ulcerative colitis
New treatment may reverse coeliac disease
IBD prevalence 3 times higher than estimated and expected to rise
Microbiome and Microbiota
Early stages of gastric metaplasia: molecular profiling
Plant-based foods and Mediterranean diet associated with healthy gut microbiome
Antibiotic resistance in H. pylori has doubled over last 20 years
Pancreatitis
New model predicts recurrence of acute biliary pancreatitis
Hepatology
Restrictive strategy for cholecystectomy selection does not reduce pain, but does reduce surgery
β-blockers may halt cirrhosis progression: PREDESCI trial
Obeticholic acid prevents liver fibrosis from NASH
Oncology
Metal stents are better than plastic for endoscopic biliary drainage
Ramosetron relieves low anterior resection syndrome
Immunonutrition during neoadjuvant oesophagogastric cancer therapy: no benefit
Endoscopy
EUS-guided histological specimens from the pancreatic cyst wall
Digital single-operator cholangioscopy more sensitive than endoscopic retrograde cholangiopancreatography
New single-use duodenoscope well-liked by endoscopists
Related Articles
October 23, 2019
Global burden of digestive diseases reveals alarming trends
October 23, 2019
Ustekinumab is safe and effective in ulcerative colitis: 2-year data
October 23, 2019
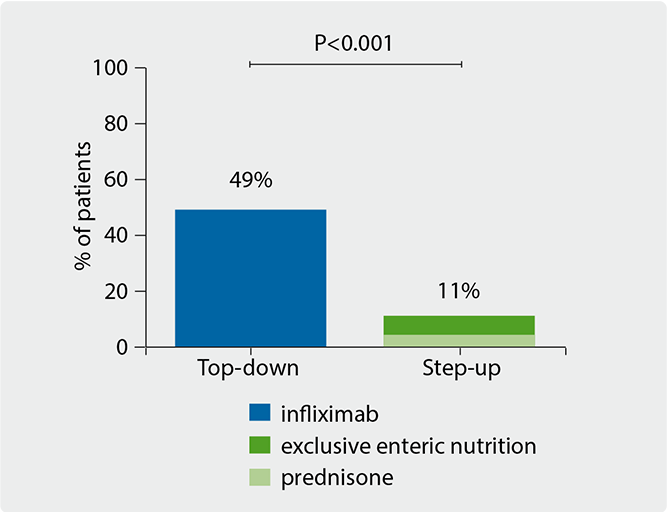
Practice-changing: infliximab in children with Crohn’s
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

