Prof. Magdy El-Salhy (Haukeland University Hospital, Norway) reported high rates of clinical response and marked symptom improvements in a large cohort of patients with various subtypes of IBS [1]. The investigators used several novel methodologies, and highlighted the importance of donor selection for optimising the effectiveness of FMT as a treatment for IBS by using frozen samples from a single 'super-donor' on individuals in the current study.
"We set out to optimise our chances of treatment success by selecting a single, well-defined donor who fulfilled European guidelines for FMT donors, and who had a favourable faecal microbial profile," Prof. El-Salhy explained.
The study randomised 164 individuals with IBS and moderate-to-severe IBS symptoms to receive either 60 g placebo solution (derived from the patient’s own faeces), a 30 g donor transplant solution, or a 60 g transplant solution. Unlike in previous studies, the transplant material had been stored frozen (-80°C/-112°F), and was administered into the proximal duodenum with a gastroscope after thawing. This approach avoids the need for bowel preparation prior to transplantation, thereby making it more amenable to daily clinical practice. The primary efficacy endpoint of the study was the percentage of patients who achieved a 50-point reduction in IBS-Symptom scoring at 3 months after FMT.
A response to FMT treatment was observed in 23.6% of individuals who received placebo, 76.9% of individuals who received a 30 g transplant, and 89.1% of individuals who received a 60 g transplant. Clinically significant symptom improvement (i.e. a reduction in IBS-SSS) occurred in 5.5%, 35.2%, and 47.3% of individuals in the placebo, FMT 30 g, and FMT 60 g treatment groups, respectively. Significant improvements in fatigue (Fatigue Assessment Scale) and quality of life (IBS-Quality of Life instrument) were also observed in the FMT treatment groups compared with the placebo group. An analysis of faecal bacterial profiles showed changes in the abundance of different bacteria in the two FMT groups, but not in the control group.
Adverse events after FMT occurred in about 20% of patients and were mild and self-limiting gastrointestinal symptoms such as abdominal pain, diarrhoea, or constipation, usually occurring intermittently in the first 2 days following FMT.
Prof El-Salhy and colleagues believe this study confirms that FMT is an effective treatment for IBS, but stress the importance of using a “super-donor” to achieve treatment success. The use of frozen faeces eliminates the logistical problems associated with FMT involving fresh faeces, making it possible to establish biobanks for the routine use of FMT in clinical practice.
- El-Salhy M. Effects of faecal microbiota transplantation in patients with irritable bowel syndrome (IBS): a randomised, double-blind placebo-controlled study. UEG Week Barcelona, Catalonia, Spain, October 19-23, 2019, Abstract OP004.
Posted on
Previous Article
« New model predicts recurrence of acute biliary pancreatitis Next Article
Decreased microvilli length in CD patients »
« New model predicts recurrence of acute biliary pancreatitis Next Article
Decreased microvilli length in CD patients »
Table of Contents: UEGW 2019
Featured articles
Interview with UEG President Prof. Paul Fockens
Upper GI Disorders
Locally active corticosteroid promising in eosinophilic oesophagitis
First-in-human radiofrequency vapor ablation in Barrett’s oesophagus
Irritable Bowel Syndrome
Faecal microbiota transplantation is effective for irritable bowel syndrome
Human milk oligosaccharides improve IBS symptoms
Inflammatory Bowel Disease
Ustekinumab is safe and effective in ulcerative colitis: 2-year data
Decreased microvilli length in CD patients
Phase 2 data shows benefit for mirikizumab in CD patients
Subcutaneous ustekinumab as maintenance therapy in UC
First evidence of long-term efficacy of ABX464 in ulcerative colitis
New treatment may reverse coeliac disease
IBD prevalence 3 times higher than estimated and expected to rise
Microbiome and Microbiota
Early stages of gastric metaplasia: molecular profiling
Plant-based foods and Mediterranean diet associated with healthy gut microbiome
Antibiotic resistance in H. pylori has doubled over last 20 years
Pancreatitis
New model predicts recurrence of acute biliary pancreatitis
Hepatology
Restrictive strategy for cholecystectomy selection does not reduce pain, but does reduce surgery
β-blockers may halt cirrhosis progression: PREDESCI trial
Obeticholic acid prevents liver fibrosis from NASH
Oncology
Metal stents are better than plastic for endoscopic biliary drainage
Ramosetron relieves low anterior resection syndrome
Immunonutrition during neoadjuvant oesophagogastric cancer therapy: no benefit
Endoscopy
EUS-guided histological specimens from the pancreatic cyst wall
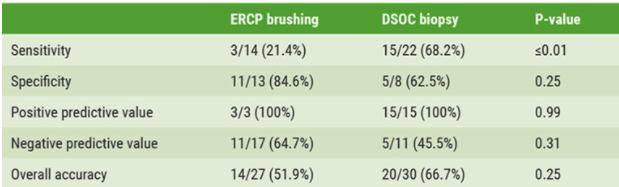
Digital single-operator cholangioscopy more sensitive than endoscopic retrograde cholangiopancreatography
New single-use duodenoscope well-liked by endoscopists
Related Articles
October 23, 2019
Metal stents are better than plastic for endoscopic biliary drainage
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

