- PBT434 demonstrated approximately proportional pharmacokinetics up to 300 mg in a randomised, double-blind, placebo-controlled first-in-human study [1]. A total of 18 healthy volunteers received oral single ascending doses (n=8) or multiple ascending doses (n=10) of PBT434. The treatment was well-tolerated. Adverse events were mild and infrequent; no serious adverse events were reported. The authors concluded that PBT434 has potential for treating synucleinopathies such as Parkinson’s disease and multiple system atrophy.
- Opicapone is a novel, highly selective, peripheral COMT inhibitor under development as an adjunct therapy to levodopa for Parkinson’s disease with motor fluctuations. In two international placebo-controlled phase 3 studies (BIPARK-1 and BIPARK-2), once-daily opicapone increased ON time without troublesome dyskinesia in this category of patients [2]. In both studies, opicapone 50 mg was associated with a significant increase from baseline to week 14/15 in absolute ON time without troublesome dyskinesia versus placebo (P=0.002 and P=0.025 for BIPARK-1 and BIPARK-2, respectively). These improvements were sustained in long-term extension studies. In the pooled safety population (n=631), dyskinesia was reported in 17.4% and 6.2% of patients in the opicapone and placebo group, respectively; rarely resulting in discontinuation.
- Once-daily venglustat at 3 escalating doses was tested in 17 Parkinson’s disease patients with a GBA mutation and symptoms ≥2 years in part 1 of the MOVES-PD trial [3]. Participants were randomised to placebo (n=4) or venglustat (n=13). All patients except 1 in the venglustat group reported at least 1 treatment-emergent adverse event; most were mild or moderate and resolved without corrective treatment during the study. The most common were psychiatric, neurological, and gastrointestinal events. No serious adverse events or deaths occurred. Dose-dependent plasma and CSF exposure were observed. CSF glucosylceramide (GL1) decreased 74.3% (high dose). Part 2 of MOVES-PD is ongoing.
- SYN120 was shown to improve cognition in preclinical models. In a phase 2a study, safety and preliminary efficacy of SYN120 in patients with Parkinson’s disease dementia were evaluated [4]. Eligible patients were randomised to SYN120 100 mg daily or placebo; they all used a cholinesterase inhibitor as well. There were 36 and 41 patients in the modified intention-to-treat groups of SYN120 and placebo, respectively. SYN120 did not improve cognition in patients with Parkinson’s disease dementia, but it may have improved cognition-based daily function. SYN120 was generally well-tolerated. Adverse events were experienced by 74% and 77% of participants in the SYN120 and placebo group, respectively; 11% (in both groups) were serious. A worsening of motor symptoms was observed.
- A survey of Parkinson’s disease patients in a medical cannabis program in the USA confirmed that medical cannabis, typically in combination with other Parkinson’s disease therapies, is a well-tolerated option to improve both motor and non-motor symptoms [5]. Medical cannabis may be helpful in relieving some adverse events of Parkinson’s disease medications, such as nausea and insomnia. Of 63 participants, 77% reported improvement in motor symptoms, most commonly tremor and spasticity; improvements in rigidity, gait instability, dyskinesia, and bradykinesia were also found. Over half of the Parkinson’s disease patients had improvements in non-motor symptoms, including sleep disturbance, anxiety, depression, and nausea. Adverse events included somnolence, disorientation, and dizziness, with 6.4% discontinuing due to adverse events.
1. Stamler D, et al. AAN 2019, S4.001.
2. LeWitt P, et al. AAN 2019, S04.004.
3. Fischer T, et al. AAN 2019, S4.002.
4. Fernandez HH. AAN 2019, S4.005.
5. Myers B, et al. AAN 2019; P2.8-016.
Posted on
Previous Article
« Biotin, ocrelizumab, and ibudilast in progressive MS Next Article
Lasmiditan: rapid onset of efficacy in acute migraine »
« Biotin, ocrelizumab, and ibudilast in progressive MS Next Article
Lasmiditan: rapid onset of efficacy in acute migraine »
Table of Contents: AAN 2019
Featured articles
Letter from the Editor
Interview with Prof. Natalia Rost
Alzheimer's Disease and other Dementias
Amyloid PET in cognitively impaired patients
Tight blood pressure control lowers risk of mild cognitive impairment
Epilepsy
Headache and Migraine
Multiple Sclerosis and NMOSD
Immune tolerance by peptide-loaded tolerogenic dendritic cells
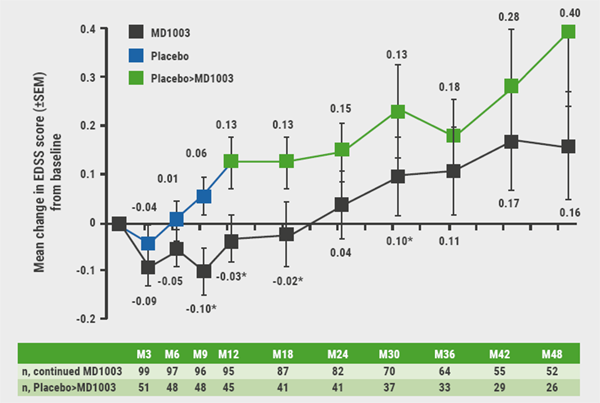
Biotin, ocrelizumab, and ibudilast in progressive MS
No increased MS relapse risk postpartum
Neuromuscular Disorders
First-ever effective and safe treatment of CMT1A
Parkinson’s Disease and other Movement Disorders
Leukaemia and hypertension therapies tested in Parkinson’s disease
Stroke
Miscellaneous
Possibly lifesaving therapy in refractory PML
New AAN guideline for treating Tourette syndrome
Subspecialty teleneurology: feasible and highly valued
Related Articles
July 30, 2019
Updates on three treatments of spinal muscular atrophy
July 30, 2019
Two experimental antibodies reduce amyloid levels
July 30, 2019
Biotin, ocrelizumab, and ibudilast in progressive MS
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

