Aducanumab (previously known as BIIB037) binds to both soluble and insoluble aggregated forms of amyloid-beta (Aβ), including oligomers, protofibrils, and fibrils. Results from the long-term extension (LTE) of the phase 1b PRIME study were presented. In patients with prodromal AD and mild AD dementia treated with aducanumab, amyloid plaque levels continued to decrease over 36 or 48 months [1]. Analyses of clinical endpoints suggested continued benefit. The safety profile of aducanumab remained unchanged.
During the core PRIME study, patients were randomised to placebo or fixed-dose aducanumab (1, 3, 6, or 10 mg/kg) for 12 months. In the LTE, all patients received aducanumab (3, 6, or 10 mg/kg; fixed or titrated). Amyloid plaque levels decreased in a dose- and time-dependent manner in the aducanumab groups over 36 or 48 months. Clinical Dementia Rating Sum of Boxes (CDR‒SB) and Mini Mental State Examination (MMSE) data suggested continued clinical benefit in patients continuing aducanumab in the LTE. Since the start of PRIME, 46 of 185 (25%) patients dosed with aducanumab experienced amyloid-related imaging abnormalities – oedema (ARIA-E), which was asymptomatic in 61%. Symptoms associated with ARIA-E were typically mild to moderate in severity. The clinical and imaging characteristics of recurrent ARIA (n=8) were typically asymptomatic. The authors concluded that these data continue to support investigation of aducanumab in the ongoing phase 3 trials ENGAGE and EMERGE.
Gantenerumab is a fully human IgG1 antibody that binds to a conformational epitope on Aβ fibrils. It has demonstrated high levels of amyloid reduction on PET scans in AD patients. In the extension of the SCarlet RoAD and Marguerite RoAD studies, high-dose gantenerumab was consistently associated with large amyloid reductions in both ARIA-E and non-ARIA-E groups of AD patients [2].
Gantenerumab was given at titrated subcutaneous doses of ≤1,200 mg monthly. Of 373 RoAD patients in the extension period, 30.6% had ARIA-E. Among 67 patients scanned after 1 year, 28 (41.8%) experienced ARIA-E; of these, 7 (25%) were symptomatic. Both patients with and without ARIA-E showed large amyloid reductions: overall -38 and -59 centiloid after 1 and 2 years, respectively. There were no significant differences between the ARIA-E and non-ARIA-E groups. However, the investigators frequently noted regional focal reductions in ARIA-E patients.
1. Castrillo-Viguera C, et al. AAN 2019, S9.009.
2. Klein G, et al. AAN 2019, S9.007.
Posted on
Previous Article
« New compounds for MS treatment Next Article
First-ever effective and safe treatment of CMT1A »
« New compounds for MS treatment Next Article
First-ever effective and safe treatment of CMT1A »
Table of Contents: AAN 2019
Featured articles
Letter from the Editor
Interview with Prof. Natalia Rost
Alzheimer's Disease and other Dementias
Amyloid PET in cognitively impaired patients
Tight blood pressure control lowers risk of mild cognitive impairment
Epilepsy
Headache and Migraine
Multiple Sclerosis and NMOSD
Immune tolerance by peptide-loaded tolerogenic dendritic cells
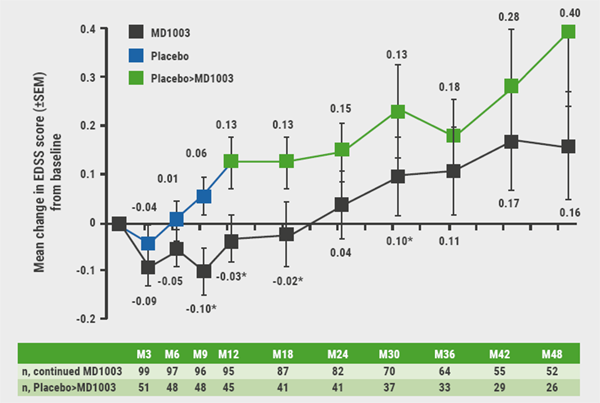
Biotin, ocrelizumab, and ibudilast in progressive MS
No increased MS relapse risk postpartum
Neuromuscular Disorders
First-ever effective and safe treatment of CMT1A
Parkinson’s Disease and other Movement Disorders
Leukaemia and hypertension therapies tested in Parkinson’s disease
Stroke
Miscellaneous
Possibly lifesaving therapy in refractory PML
New AAN guideline for treating Tourette syndrome
Subspecialty teleneurology: feasible and highly valued
Related Articles
July 30, 2019
Biotin, ocrelizumab, and ibudilast in progressive MS
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

